MEDEX Northwest has been helping veterans enter the PA profession since its inception in 1969. The original goal to leverage military medical training and experience for a civilian PA career remains a key part of the MEDEX mission. This program accepts and educates the highest percentage of military veterans among civilian PA programs. With years of experience integrating veterans into the classroom, and having faculty who are also veterans, MEDEX is uniquely positioned to help veterans be successful in the transition into civilian life.
With the 2018 incoming class fully 25 of the 135 new students, or 19% of the cohort, come from a military background. The breakout is as follows: 11 Army, 7 Air Force, 4 Navy, 2 Marines and 1 Coast Guard.
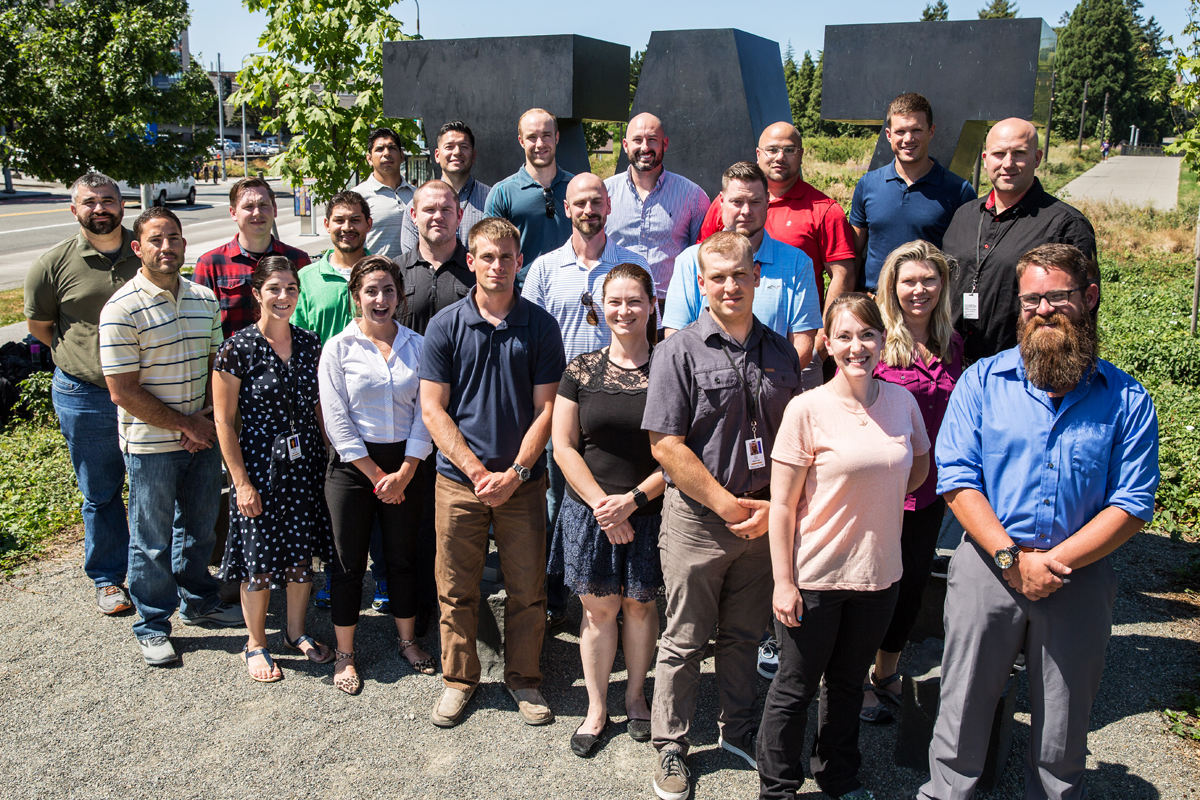
On Tuesday, August 7, all 25 veteran students from the 2018 incoming class met for a veteran benefits orientation to learn about accessing various benefits available to them while attending MEDEX at the University of Washington.
Tina Tanaka of the UW Veterans Office explained how these individuals could maximize their GI Bill benefits and other services. They also learned about various sources for scholarship funds through the national American Academy of Physician Assistants (AAPA) Veterans Caucus, the local Washington Academy of Physician Assistants (WAPA) Veterans Committee, and MEDEX itself. There is a wealth of support available to any veteran student looking to pursue these channels.
We’d like to introduce you to two of the veteran students from the 2018 incoming class. Their individual stories are representative of the wide-ranging experiences among all the MEDEX veteran students.
Coty Holm – Spokane Class 22
Coty Holm makes his home in Bozeman, Montana, although he’s lived in a lot of different places while following his father through medical school.
“We lived in Portland for quite a while my father was doing his undergrad at PSU (Portland State University) and his medical studies at OHSU (Oregon Health & Science University),” says Coty. Later, his father did a residency in North Dakota. “So, I did most of my high school a little way outside of Minot, ND.”
The senior Holm graduated from medical school when Coty was 14 years old. “It’s a big reason why I chose the PA profession,” explains Coty.

“I am married with three kids, and I know what it was like to have a parent in med school. It would take a very long time—four years in medical school. And if I want to do surgery, that’s another six years in residency. That would be ten years out-of-state because Montana doesn’t have a medical school.”
But we’re getting a bit ahead of ourselves.
During his senior year in high school, Coty got his EMT license in Washington State. Over five years he worked as an EMT firefighter for the city of Ocean Shores, WA and for Grays Harbor Fire District 7. Through it all, his 24 on/24 off schedule allowed him to take on part-time construction work.
At the end of those five years, Coty got his Washington MA license, phlebotomy certificate, and went to work in primary care for Coastal Family Medicine in Ocean Shores. Eventually, a return to Montana proved irresistible. He did more construction work and considered enrolling at MSU Bozeman before deciding to enlist in the U.S. Army.
“I had several friends in the military,” he tells us. “Plus, I wanted to enlist for the free college through the GI Bill.”
 When Coty enlisted in the Army he didn’t have a specific career goal in mind. “I just wanted to be in the Army,” he says. Because he had been an EMT, the recruiter pushed him hard to become a medic. “But I was kind of burned out on it.”
When Coty enlisted in the Army he didn’t have a specific career goal in mind. “I just wanted to be in the Army,” he says. Because he had been an EMT, the recruiter pushed him hard to become a medic. “But I was kind of burned out on it.”
Coty was hoping for an enlistment bonus but arrived at a gap in time when the bonus was unavailable. His thinking was, “If I’m going to be in the Army and I can’t get an enlistment bonus, then I want to do something that I can’t do on the civilian side.”
So, Coty went to infantry school and saw a deployment to Iraq within three months.
“I spent 12 months in Iraq,” Coty says. “My youngest son was born about a month after I deployed. We already had two kids, and then my wife had a newborn. She was by herself most of the time, so that was pretty rough on her. That was a rough year for our family.”
While in Iraq, Coty learned that his battalion had a sniper section. Towards the end of his deployment, he submitted his application for the sniper section. What followed was a two-week selection course, and then he was selected to join the section.
“I trained with them for a year, and then went to sniper school in 2014,” Coty tells us. “Ever since then, I’ve been a sniper.”
The question comes up: how does Coty go from being a sniper in the army to becoming a PA? A lot of people see those as opposites.
But for Coty, being a sniper isn’t about killing people.
“It’s about saving lives, because you’re a precision instrument,” he says. “You can remove a single threat in a town or a landscape—one person, one bomb maker, or a trigger man. And you can save many lives, from convoys to your buddies on patrol. So that’s really what it’s about for me.”
For similar reasons, he wants to become a surgeon as a PA.

“You go in and remove the tumor or a specific problem rather than bombarding the whole mass. I see a lot of correlation between the precision of a sniper and the precision of a surgeon. And I think that attention to detail, being able to deal with high-stress environments while making tough decisions during my military career, will carry over into being a PA.”
During his undergraduate years, Coty spent a number of hours with an orthopedic PA and other surgical physicians in the OR. “I like being in the OR,” he says. “I like the hands-on cutting and fixing, the challenge of it and the precision. Orthopedic surgery is very much like construction with all the drilling and hammering. I like emergency medicine and trauma—and sports like skydiving, mountaineering and motorcycles—all because of the adrenaline.”
This is in contrast to Coty’s exterior presentation, which is very calm.
“That’s probably a result of my personality and military training. I’m probably borderline OCD—very detail oriented, so I think surgery fits me well. You tend to notice a lot of things.”
Coty was part of the Montana National Guard until this past December when he was accepted into MEDEX, at which point he transferred to the Washington Guard for the duration of his physician assistant education at the Spokane site.
“I’m on inactive status while I’m attending MEDEX, so my contract is on pause,” he says. Once he graduates in late 2020, Coty will pick it up where he left off. “I’ll have three years left with the Guard.”
“I’ve done a lot of things in my 33 years,” says Coty. “None of it are the things I thought I would do, but life’s interesting that way.”
Anna Zakharova – Spokane Class 22
Anna Zakharova received her formal medical education as a corpsman in the US Navy. However, she was exposed to medicine very early in life. Born and raised in Ukraine, her grandfather was a doctor and her grandmother a nurse.
“I considered pursuing medicine when I was 15 or 16,” Anna tells us. She started college in Ukraine before moving to the States at age 17 and a half. “My mother married an American citizen. I came to the US a year later because I was still in school.”
Later, her grandmother and an aunt followed.

There were adjustments to be made. “My mom was an English teacher back in Ukraine, so I learned English from an early age,” she tells us. “Language wasn’t an issue, but the culture was different.”
It took Anna about a year to obtain her green card. With that in hand, she enlisted in the Naval Reserve and trained to become a corpsman.
“Yeah, I’m still a reservist,” she explains. “I was mobilized for the past two years.” In fact, Anna just got off active duty a week and a half before starting the MEDEX program with Spokane Class 22.
Originally stationed with a marine unit in Camp Pendleton, CA and then Miramar, CA, Anna was deployed in 2017 for 7 months. “We were part of the Special-Purpose MAGTF AFRICOM-Crisis Response, but we were stationed out of Spain.”
She explains that the team was part of the USMC task force established to respond to different crises in a specific area of Africa.
“My squadron flies V22 Ospreys and our job was to fly in to pick up or deliver and then to fly back. The primary focus was casualty evacuation, if we were ever needed. If we had casualties to pick up, or if we needed to go for supplies, we would pick them up and deliver them wherever it was needed.”
Casualty evacuation was not a regular event, so in the course of her duties, Anna was treating mostly young and healthy patients. “These were marines who had hurt themselves or gotten sick,” she says. “Primarily, it was normal day-to-day stuff.”
 When not on active duty, Anna also had a civilian job. For the past five years she’s been working at the VA as a nursing assistant.
When not on active duty, Anna also had a civilian job. For the past five years she’s been working at the VA as a nursing assistant.
“There I had more exposure to post-military veterans, including Vietnam Era veterans,” she says. “They tend to be a little bit different from the general population. Some were exposed to Agent Orange, so they had a lot of health issues.” Diabetes and emphysema played a big role. She saw patients that had cancers, and diseases that go hand-in-hand with drugs, alcohol abuse and smoking. “These are often the results of more self-destructive behaviors.”
Looking ahead to the future and her new profession as a physician assistant, Anna has some definite ideas about how she might contribute to her fellow veterans.
“I’ve always been interested in psychology,” she says. “It started out because I had friends coming back from Iraq and Afghanistan that were suffering from PTSD. I didn’t understand it very well, so I got my bachelor’s in psychology. I want to work with veterans and active duty personnel doing psychiatry. Because I didn’t go to Iraq or Afghanistan, I wanted to do something that was helpful in some way.”
Anna originally planned to do a PhD in clinical psychology, but that meant not practicing medicine anymore. Then she learned about the PA profession, and that both clinical psychology and a medical practice could be combined.

“I wouldn’t have to give up anything,” she says. “I’ve been told that about 50% of cases in the emergency room and primary care have some kind of psychological issue.”
That’s her favorite part of becoming a PA. “It’s very flexible. You can go from one specialty to another much more easily than in any other profession in medicine. So, I’m probably going to do something with psychiatry. Of course, I want to explore other specialties too and see what else might interest me, but I think emergency medicine and psychiatry are the two big ones. It’s what most of my training has been.”
Anna is a big on fitness and is a Zumba enthusiast. “Exercise is important to me,” she says.
Three or four years ago at the VA she had to do CPR compressions on a 300-pound man. “I’m pretty small,” she says. “So, the next day my arms felt like they were going to fall out of their sockets—like somebody tried to rip my arms out. I realized that it’s not just about your knowledge. A big part of the job is also physical. You have to be physically ready to do certain things for patients, like CPR. If you’re not physically fit yourself, you can’t really help somebody else.”