Each summer, MEDEX Northwest welcomes its incoming class to the physician assistant education program. Students from all four sites—Seattle, Spokane, Tacoma and Anchorage—converge on the University of Washington campus in Seattle for six weeks of instruction and bonding before they go to their separate sites for the remainder of the year.
Of course, they all had been working their online Anatomy & Physiology course since March, but July 2nd 2018 was the first time the 135 students came together under one roof. There is a rush of excitement as the individuals collected their information packets and changed into their purple MEDEX t-shirts, then took their seats in the auditorium for Day 1 Orientation.
Founded fifty years ago by an African American MD, Dr. Richard A. Smith, MEDEX Northwest has a long history of recruiting a diverse set of student candidates to its program. But this year is a new milestone. Fully 31.9% of the 2018 incoming students are racial minorities.
MEDEX Program Director Terry Scott, MPA, PA-C, DFAAPA, believes this is critical for the future of healthcare delivery in the U.S.
“As our nation becomes more diverse, it’s important for us to have providers who look like and are from the communities in which they serve,” he says. “My hope that this is just the beginning, because I think that we should continue to recruit a diverse set of candidates to our program.”
What’s so impressive is that MEDEX achieved this without any federal or state funds.
“We did this in an environment prohibiting the use of race and other characteristics in the admissions process,” adds Scott. “Institutions receive millions of dollars in grants with the agreement to pursue diversity initiatives, and they don’t get these results.”
Scott contends that diversity should be a cause.
“In reality, we should be doing this because it’s the right thing to do,” he adds. “It’s our commitment to diversity and inclusion that has resulted in these numbers. We actually have it as a value.”
He’s also quick to add that these numbers didn’t happen overnight.
“I think it’s something that candidates to our program recognize, seek out and appreciate. Individuals find us because we have visibility in these areas. We’re not just giving lip service. This is something we live and breathe.”
To begin, Terry Scott is one of the few African American PA program directors in the country, as well as one of the few African American program directors within the UW School of Medicine. He’s quick to attribute responsibility elsewhere, too.
“The attempts by our Admissions Team to reach out into communities and identify strategic areas of focus are key. Our website demonstrates the diversity of our faculty. MEDEX Magazine and our videos tell the unique stories of our students. All this took several years to bear fruit.”
From the start, MEDEX was founded as a way to bring medically trained military veterans into public sector healthcare jobs. And today, veterans play an important part in MEDEX—faculty, staff and students. 19 percent of the 2018 incoming students are military.
“This is another important piece for us because our veterans deserve an opportunity to come back and have a better-than-living-wage job opportunity,” says Scott. “That’s what this program and the PA profession affords.”
Terry Scott wants those who are considering PA education to sit back and ask, “What kind of program do I want to apply to? Do I want one with values similar to my own? Can I see people that look like me? Do they have stories that I can relate to?”
“When that happens, it’s a beautiful thing to observe,” he says.
We’d like to share some of the unique personal stories from a handful of students comprising the incoming MEDEX Class of 2018.
Lauren Trew – Spokane Class 22
 Lauren Trew admits that her path to medicine is a convoluted one.
Lauren Trew admits that her path to medicine is a convoluted one.
She received her undergraduate and master’s degrees in music, and worked initially as a music educator for the Seattle Symphony, and then as a music librarian for the Alabama Symphony in Birmingham, AL. She also plays woodwinds and sings.
“When I worked in music full time, I realized it took some of the joy out of music,” she tells us. “I didn’t feel like I was doing anything extraordinary or unique.”
And so, Lauren came back to hometown Seattle, and looked at what other options were out there. She learned about medical assisting and dipped her toes in the water. “I got my medical assisting certificate and tried that out, and then learned more about other roles in medicine.”

As an MA at the University of Washington Medical Center, Lauren worked with PAs and nurse practitioners, and decided to become a medical provider in that same capacity. From there it was a matter of pursuing the necessary prerequisites, and applying to MEDEX.
Initially a candidate for the MEDEX Seattle cohort, Lauren finally placed with Spokane Class 22. “I’m not dead set on coming back to Seattle necessarily, but I love the area,” she tells us. “I’ve had some amazing experiences working with the LGBT community, especially with transgender patients. I’ve had the opportunity to work with some primary care providers who are really addressing the concerns of that community at a higher level. And it’s good to see the progress there. I think I’d like to be a part of that and help out those folks because they do have different needs than your average patient.”
As a musician and trained singer, we wonder if Lauren can be counted on to lead her class in show tunes.
“Oh, dear. Is that a test that we have? Because I’ll definitely ace that one.”

Hiep Nguyen – Seattle Class 52
 “On this, my first day, my impression is … I’m loving it,” say Hiep Nguyen. Looking around the crowd of 135 new incoming PA students, he’s positively gushing. “Everybody here feels like they want to be here. They’re happy, smiling and excited. It makes me excited too. It’s not just about the program, it’s about the people that are going to be my family for the next two years.”
“On this, my first day, my impression is … I’m loving it,” say Hiep Nguyen. Looking around the crowd of 135 new incoming PA students, he’s positively gushing. “Everybody here feels like they want to be here. They’re happy, smiling and excited. It makes me excited too. It’s not just about the program, it’s about the people that are going to be my family for the next two years.”
It’s clear that Hiep is destined to become something of a cheerleader for his class. He’s brimming with enthusiasm and positive energy.
“Yeah, I have a big heart even though I’m a small guy. I love working with the homeless community. I actually just came back from a mission trip to LA. It’s the densest area for homelessness. There are tons of organizations that help them, but not necessarily enough hands to work with the homeless community down there. So, I went down there, took a bunch of high school kids with me, and we just served in whatever way was needed.”

Hiep took the youth into the streets, talked to people, gave them their time and food. “We served 3,000 meals,” he says. “We talked and smiled, telling them that they matter and are important. Even though there was some negativity, a smile goes a long way. It was really fun.”
Prior to entering the MEDEX program, Hiep did five years of clinical research right here at the University of Washington with a focus on prostate and bladder cancer research.
“I work with the patients across the different departments that are involved in new therapies, like ophthalmology and radiology,” he explains. “I’m the center of the spider web making sure that patients get treated not only for their cancer, but are involved with the research too.”
Hiep splits his time between the Prostate Oncology Clinic over at the UWMC surgery pavilion and the Seattle Cancer Care Alliance. “That’s where we see most of our patients,” he explains. His five years of medical experiences have had him working in clinical settings with patients and following around doctors, PAs and nurses.
We wonder if his future as a physician assistant lies in oncology.
“Well, I do have a bias towards oncology because I know the terminologies,” he says. “I know what these patients are like. But I kind of want to expand my horizon a little bit. Maybe one day I’ll return to oncology. I’m just really open about all the possibilities out there and I’m really excited to learn a lot.”
Kusuma Ayithepalli – Tacoma Class 6
 Entering into a career in the US healthcare system is challenging enough for someone who is native born. It’s much more so for someone educated in a system outside this country. For International Medical Graduates (IMGs), there is the USMLE, or US Medical Licensing Examination, in order to determine equivalency and the educational path forward. The process is complicated, which is why some IMGs turn to the accelerated pathway of PA education.
Entering into a career in the US healthcare system is challenging enough for someone who is native born. It’s much more so for someone educated in a system outside this country. For International Medical Graduates (IMGs), there is the USMLE, or US Medical Licensing Examination, in order to determine equivalency and the educational path forward. The process is complicated, which is why some IMGs turn to the accelerated pathway of PA education.
Kusuma Ayithepalli started her post-graduate education as a junior resident in India, wishing to become OB/GYN physician in her native India. But she got married and followed her husband to the US for his work.
“I came over here, and it was very new,” she tells us. “I hadn’t planned on coming here before. It took me a year to become acquainted with the US system and to plan my career.”
Two children soon followed.
Kusuma started preparing for the USMLE and Medical Boards. She took on a residency rotation for the experience and to learn how the United States healthcare system works. Halfway through that rotation she met a physician assistant on duty.
“In India there are no PA programs. So, I was really interested and started exploring more about the PA program. I decided that this would be a better fit for me to achieve my dream.”
At that point, Kusuma began focusing on what to do next. Her educational counselor at Edmonds Community College directed her toward the necessary prerequisites, and she attended a MEDEX information session.
In order to gain the requisite patient hours for admission to a PA program, Kusuma went ahead and received several medical certifications—as a lab assistant, in phlebotomy, a nursing assistant and an EKG technician. “I did all that is needed for the PA program, and then I started applying for the programs.”
While in the process of completing her US Equivalency Boards, she realized that most of the opportunities for IMGs were focused on the East Coast of the United States. “There is some kind of percentage for acceptance” she tells us. “There are more opportunities and programs there compared to Washington State. I couldn’t go to the East Coast leaving my two kids and family here.”
Now a part of the Tacoma 6 cohort, Kusuma can look ahead past her graduation in August of 2020.
“I imagine myself practicing in primary care,” she says. “I like interacting and being an advocate for people, and the PA program offers a good scope of practice and flexibility. I really like the program. I might go into like GI or cardiology later on. Those are my two areas of interest.”
But not back to OBGYN, we ask?
“OBGYN, no,” she replies. “It’s been a tough journey, but I made it.”
Mikayla DeSoto – Anchorage Class 10
 A native of Naknek, Mikayla DeSoto may come from the smallest community among her entire Alaskan cohort. “Wikipedia puts the population at about a thousand,” she says. “Personally, I feel it’s less.” She’s also well aware of the healthcare challenges posed to people in the remote areas of Alaska.
A native of Naknek, Mikayla DeSoto may come from the smallest community among her entire Alaskan cohort. “Wikipedia puts the population at about a thousand,” she says. “Personally, I feel it’s less.” She’s also well aware of the healthcare challenges posed to people in the remote areas of Alaska.
“Many are afraid to go to clinic because they’ve had bad experiences,” she says. In a land of itinerant healthcare workers, Mikayla feels like it’s difficult to build long term relationships with providers. Sometimes people will avoid care altogether because they think they’re not sick enough or are incurable.

But Mikayla is optimistic. Her home is Naknek, and her family members reside there as well. She understands how important it is to build trust through relationships in a small community, and expects to practice as a PA in rural Alaskan villages. “I would love to work for a long period of time in my community, to kind of give back for what they’ve done for me,” she says. “Once that relationship is bonded, it grows and things will get better.”
Prior to MEDEX, Mikayla worked as a medical assistant at Camai Community Health Center in Naknek. Originally focused on the nursing pathway, she found it highly competitive. “If you didn’t get 100 on your tests or 4.0, you were unlikely to get in. I didn’t have a bad GPA. But here at MEDEX, they want to know who you are and if you can rise to the occasion. I’m very excited for the things to come.”
Gavin Dawson – Spokane Class 22
 Following his graduation from the University of Colorado, 22-year old Gavin Dawson was first exposed to physician assistants while working for Wilderness Medical Associates, a wilderness medicine training organization in SE Asia. He worked with a team of medical professionals to train individuals or companies practicing in remote and austere environments.
Following his graduation from the University of Colorado, 22-year old Gavin Dawson was first exposed to physician assistants while working for Wilderness Medical Associates, a wilderness medicine training organization in SE Asia. He worked with a team of medical professionals to train individuals or companies practicing in remote and austere environments.
“If something goes awry, and you’re away from the hospital,” he explains, “what can you do? Can you keep this person with a traumatic injury alive in the field, or do they need to get out now? We gave those trainings all over Southeast Asia.” Wilderness Medical Associates teaches on all seven continents, in fact.
Some of the most influential instructors Gavin worked with, and some of his best friends, were PAs. “They liked me because I had an integrative physiology and neuroscience background, along with the wilderness EMT component,” he says.
Over the course of five years at Wilderness Medical Associates, Gavin learned how to teach wilderness and emergency medicine, and make this information accessible to a variety of different populations. “Our hub was based in Thailand, but we’d go to, Laos, Belize, Finland, the United States, all over, really, to train different clients.”
 All of this left Gavin with a deep passion for different cultures. “With traveling, one of things I’ve noticed is that there are some very impoverished places throughout the world,” he says. “But there are also some very impoverished places within this country as well. I feel strongly about working with that group of people and making a difference.”
All of this left Gavin with a deep passion for different cultures. “With traveling, one of things I’ve noticed is that there are some very impoverished places throughout the world,” he says. “But there are also some very impoverished places within this country as well. I feel strongly about working with that group of people and making a difference.”
This all started very young. Gavin’s mother was a Rolfer, a deep tissue physical therapist. “I grew up in an environment where I was always exposed to healthcare,” he says. “Her office was in our house so, growing up, there were always people coming in and out and doing movement therapy. That seed was planted very early on.”
Growing up in Colorado, the outdoors played a large part in Gavin’s development. “I was always going outside hiking, climbing, biking and skiing.” In college, a wilderness EMT intensive course and clinical rotations in Wyoming allowed him to finally marry his passions for the outdoors and medicine.
Back at University of Colorado Boulder, Gavin started working for CU Sports Medicine with a focus on student emergency medical services. Upon graduation, he moved to SE Asia to work for Wilderness Medical Associates.
“Wilderness medicine occupied eight or nine months of the year, but winter is my happy place,” Gavin tells us. “Usually, I’d get out of the heat and humidity, come back to Colorado in the winter and work on an ambulance, and ski.”
Looking ahead beyond MEDEX, Gavin imagines himself working in a low resource environment. “Perhaps that’s a rural town. I’m still trying to figure that out.”
For the moment, he’s excited about his Spokane cohort.
“Already, we’re a really tight class,” he says. “We’ve gone to a baseball game together and are studying together. I’m excited for the teamwork aspect of this. At the end of the day, medicine is a team effort.”
Penny Pukall – Seattle Class 52
 Penny Pukall was an AMR paramedic on the scene of the October 1st 2017 mass shooting on the Las Vegas Strip. Between 10:05 and 10:15 pm, a single gunman fired at the Route 91 Harvest Music Festival, resulting in 58 fatalities and 851 injuries.
Penny Pukall was an AMR paramedic on the scene of the October 1st 2017 mass shooting on the Las Vegas Strip. Between 10:05 and 10:15 pm, a single gunman fired at the Route 91 Harvest Music Festival, resulting in 58 fatalities and 851 injuries.
“It was chaotic,” Penny says. “But it was amazing at the same time, because EMS, fire, and the hospitals—we all worked together. The teamwork that night was insane. So many people came in on their day off, just came in. We literally took every single ambulance that we had at AMR, even the out-of-service ones where, say, the AC didn’t work.”
Penny noticed that inter-departments that usually scuffle between one another—like fire and police—set aside differences to work together. “Even those people who weren’t EMS, they went in to help. It was crazy. Uber drivers were on standby, even though they were at the greatest risk.”
“It’s just crazy to look back at it. No one was fighting. Everyone was there to help and that was cool. It made me a better person.”
At age 19, Penny moved to Las Vegas from her home in Wisconsin. “I thought, where is there no snow? Which is kind of funny because my favorite thing to do in the world is snowboarding. I just didn’t want to live in it.”

In Las Vegas she discovered EMS through some friends and started working as an EMT and then a paramedic. She put in seven years with AMR. Early on, Penny discovered the limitations of her job.
“On my ambulance, I have 10 things I can do,” she says. “It’s literally a guessing game. I can hear lung sounds and like, ‘Okay, well, it sounds like rales, so I’m going to treat it with this,’ or, ‘You have a history of asthma? We’re going to go with this.’ Still, I only have about 10 things in my ambulance to treat that patient. There’re so many more other options out there that, if I had different skills, I could do so much more.”
Clearly, paramedic training wasn’t enough for Penny. Right after paramedic school, she started working on her bachelor’s degree and pre-requisites in order to qualify for PA school.
Penny went to her MEDEX admissions interview two weeks after the October 1st Las Vegas shooting.
Now in Seattle as part of Class 52, Penny is freezing. “It’s so cold here,” she exclaims. “Las Vegas was 110 degrees when I left. Here it’s 62, and I was like, ‘Where’s my jacket? Do I even own a jacket?’”
In order to make the move, Penny sold everything. “I have a mattress and about six boxes that I fit in this tiny little U-Haul. And my Jeep, I love off-roading. I take my Jeep everywhere, and I have a dog named Molly. She’s a 90-pound big fluffy white Samoyed.”
Looking ahead to the future, Penny is open to whatever comes her way. “If I get a cool clinical rotation up in Alaska, I’m all for staying. I am so open right now. Vegas is cool. I have a lot of friends there and can always go visit. But if I get a really cool clinical somewhere and I fall in love, I’ve sold everything so that I can go anywhere.”
Scott Peckenpaugh – Tacoma Class 6
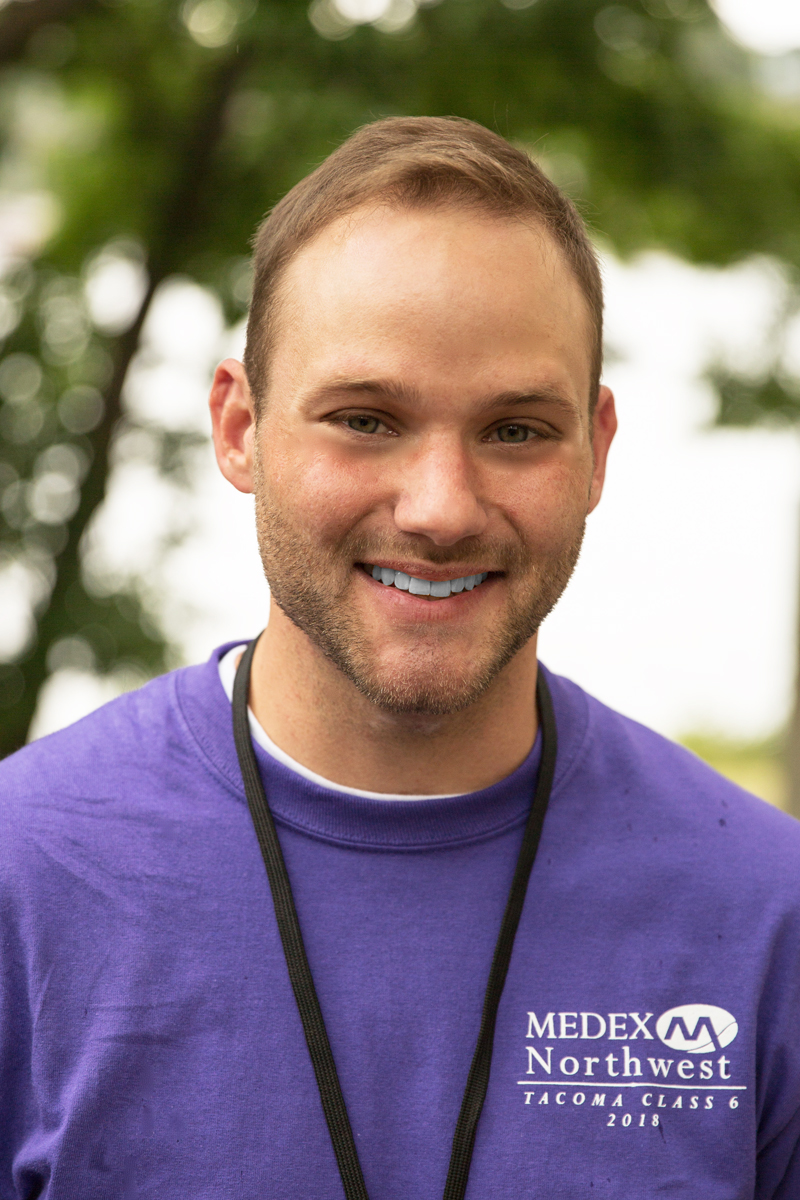 With almost eight years as an ER tech, and a total of 12 years in emergency medicine, Scott Peckenpaugh comes to MEDEX Northwest with well above the requisite 2,000 hours of hands-on patient contact. He started young.
With almost eight years as an ER tech, and a total of 12 years in emergency medicine, Scott Peckenpaugh comes to MEDEX Northwest with well above the requisite 2,000 hours of hands-on patient contact. He started young.
“By the age of 18, I got my Emergency Medical Technician certification,” Scott tells us. “I was affiliated with the fire department for a little while, doing EMS in the Silverdale area of Central Kitsap County.”
In time he moved away from seeking a career in the fire service and started working for a private ambulance service. “I was digging through patient charts, doing these inter-facility transports and really gained a deep appreciation for the puzzle that is medicine.”
During this period Scott noticed the way that PAs developed connections with their patients. “They treat their patients as a person rather than just a sprained ankle in Room 12, and I found that very unique. So, I began to self study a bit and worked myself up to the point where I realized after working as an ER tech that the PA route was the way I wanted to go. And here I am today.”
Scott has a vision of bringing primary care to everyone, which is one reason the MEDEX Northwest program resonated with him.

“I was born and raised in Washington State,” he says. “I’m so proud that MEDEX is from my home state. I researched a lot of different PA programs, and MEDEX just aligns so closely with the idea of patient-centered care. That’s one of the reasons why I am proud to be here.”
Scott volunteered at West Sound Free Clinic in Bremerton, WA. One of the things he noticed was that the patients were coming from the Bremerton proximity and no further. “Every day the line was 20 to 30 deep just to be seen for basic medical services that could be taken care of with preventative medicine and follow-up primary care.”
So Scott began to ponder, why not take this out to the wider community, make it mobile, go where it’s needed? “We could gather information from different communities on what’s needed, coordinate the right amount of care, and network with local establishments to figure out what charitable care we can offer so that everybody can have access.”
Clearly, Scott is a person of vision. He’s even aware of the MEDEX Tacoma Foot Project, a monthly didactic student outreach project providing basic foot care and important medical referrals to the homeless community.
“I plan to take part in that,” he says with a smile.
Yanet Medina Chinas – Anchorage Class 10
 A medical doctor in her native Mexico, Yanet Medina Chinas fled to the United States in 2013 due to domestic violence. After 18 months in the US, she officially received asylum. The only place she could go was Anchorage. “It’s a long way, but my brother was living there.”
A medical doctor in her native Mexico, Yanet Medina Chinas fled to the United States in 2013 due to domestic violence. After 18 months in the US, she officially received asylum. The only place she could go was Anchorage. “It’s a long way, but my brother was living there.”
From 2009 to 2013 Yanet had practiced as a public medicine physician in Mexico. However, gaining the medical equivalency in the US proved difficult.
“It’s is a big challenge when you come to this country,” she tells us. “I failed at obtaining some of the equivalent credentials. I decided to quit medicine and started working as a janitor and maid.”
Now able to legally work, she started cleaning buildings in Anchorage. In a situation where many would have felt crushed or defeated, Yanet kept a positive mind set. “Whatever you do, you have to do it right. It didn’t matter if I had to clean buildings. I set my goals to clean them better, faster, and just stay positive about what I was doing.”
But as years started passed, Yanet started missing medicine.
She looked into the Nursing Assistant program at UAA—the University of Alaska Anchorage. She thought, “Well, maybe I can get a scholarship and be a nurse assistant and take blood pressure.” When Yanet’s advisors learned of her extensive medical background, they redirected her to the MEDEX physician assistant program.
She started reading about MEDEX and the PA profession that same afternoon.
“I realized this is what I want to do,” she says. “MEDEX was committed to public health and diversity. There were many International Medical Graduates too, and people from different backgrounds. I like this.”
Now a part of MEDEX Anchorage Class 10, Yanet doesn’t expect the next two years to be an easy ride just because she’s an International Medical Graduate (IMG). “There’s still a bit of a language barrier,” she says. “I still have an accent, I still have to learn many words. When I express myself, I have to remember the things that I learned as a doctor in foreign country, and to learn them again in English. Of course, medical vocabulary is mostly the same, but still, I find it challenging.”
Like many, Yanet is distressed by the recent negative focus on immigrants to the US.
“I would like to say that United States is a place where immigrants can contribute, too. We come here, we work hard, we do our best. I started here as a janitor and a maid. We’re not taking opportunities from anybody. We come to contribute to this country. And I love this country.”
Manpreet Kaur – Spokane Class 22
 Born in the North Indian State of Punjab, Manpreet Kaur moved to United States with her mother at age five. She grew up in the Hillyard neighborhood of Spokane, WA, working at a gas station alongside her parents.
Born in the North Indian State of Punjab, Manpreet Kaur moved to United States with her mother at age five. She grew up in the Hillyard neighborhood of Spokane, WA, working at a gas station alongside her parents.
“I stocked in the back and helped out with random chores around the business,” she says.
Most of all, she observed her father helping people, and she knew that a helping profession was in her future. “I didn’t really want to work there, necessarily. I would say business isn’t the right field for me.”
Another key component of Manpreet’s background turned on her being sick a lot as a child.
“We didn’t have any health insurance. My dad would take me to a doctor. She would help us, give us free medications, and try to figure out ways to make it cheaper for us.”
Manpreet thought, “I want to be like her.” Looking at her ID card, the “doctor” turned out to be a PA. With a title to the profession, Manpreet knew the path forward. “That’s it! That’s what I want to do!”

There was a long way to go for Manpreet before arriving at her first day at MEDEX Northwest. Not quite understanding the path forward, she signed up for pre-med before her research led her to realize that physician assistant was an accelerated medical program. “Oh, this is interesting. Two years versus four years to become a provider.”
Even her pathway to becoming an ER Tech was unconventional. Manpreet started volunteering to learn more about medical careers. She was volunteering at the medical tent for Spokane’s annual Hoopfest through Holy Family Hospital when a manager pulled her aside.
“I sat down to talk with her, telling her of my desire to work in the medical field,” Manpreet says. “The whole time this manager is writing things down, asking me questions.”
“Wait, am I being interviewed?”
Turns out she was. Providence Holy Family Emergency Room hired Manpreet as an ER Tech and trained her for the job.
“Stuff just worked out,” she says with a smile.
Mission-driven and focused on providing care to the underserved–a population she once considered herself a part of–Manpreet envisions a primary care practice for herself in a rural setting.
“I also want to go back to India do some volunteer work in my village and the villages around there. In my lifetime I’ve been back there three times now for a couple of months.”

Eric King – Seattle Class 52
 At age 12, Eric King watched his father become chronically ill. As a high schooler, Eric began managing his father’s medications. It was at that early age that Eric knew he wanted to do something in healthcare later on in life.
At age 12, Eric King watched his father become chronically ill. As a high schooler, Eric began managing his father’s medications. It was at that early age that Eric knew he wanted to do something in healthcare later on in life.
He learned that pharmacy technician was something he could do right out of high school. “It came from this roundabout way of having personal experiences with my dad and later, my mom,” he says. “And I was okay at science.”
A pharmacist that Eric worked with held the dual credentials of PharmD and PA-C. “We were talking about what I wanted for my future, and that what I wanted wasn’t necessarily found with pharmacy.” Eric decided to start shadowing local physician assistants. Some of these PAs had come out of MEDEX and were working with HIV positive communities in Seattle. He decided to switch from outpatient pharmacy to inpatient, where he could see more PAs and really observe the breadth of experience and the diversity of jobs that the profession fulfills.
“Wow, they’re everywhere,” Eric recalls thinking, “and there’s nothing they can’t do.” Following these shadowing experiences, Eric knew he wanted to become a PA.

After seven years of working as a pharmacy tech, Eric decided to go back to school to become a PA. He started taking classes at a community college and began undergraduate research in the department of Neurological Surgery at the UWMC. When he transferred to the UW he had plans of continuing his neuro-oncology research projects and obtaining a bachelor’s degree in neurobiology.
A change of direction came after Eric’s first quarter as a UW student.
“I took a medical anthropology class and was introduced to public health,” he tells us. Eric switched from biology to become a public health major and received his undergraduate degree at the UW. “At that point I considered applying to PA school and then decided to continue with public health to get my master’s degree.” It was the logical next step.
“We look at illness and always say, ‘Go see a doctor,’ when really there are lots of upstream things we could do with public health to prevent it.”

In 2016 Eric was selected as the graduate student representative for the UW Population Health Initiative Executive Leadership Counsel, where he has helped shape the vision of this project. He believes his public health education and experiences with the Population Health Initiative will make him a better clinician. He received his MPH from the UW in June 2018.
As Eric looks ahead to his graduation from MEDEX in August of 2020, he has clear sights on the kind of work he wants to do as a PA.
“You know my heart is with the LGBTQ community,” he says. “I really want to work with that population. That’s how I identify. I have a strong connection and passion to HIV care through my personal and professional experiences as well as my public health education. I’ve worked with the transgender community. I really see a lot of different aspects of value and opportunities for improvement, whether it be in primary care, providing cross-sex hormones, or working with youth. I love children so that might be something to explore. But I’m definitely focused on the LGBTQ community, and using the skills obtained from my public health degrees for program evaluation/implementation or the development of health policy. I don’t see myself only doing clinical work.”
Whitney Miller – Anchorage Class 10
 Apart from her college years in North Dakota, Whitney Miller has spent her entire life in Anchorage, Alaska. “My mom is from North Carolina. She was a military brat who followed my maternal grandfather to Joint Base Elmendorf–Richardson. My dad is from Canada and got a full-ride scholarship to University of Alaska Anchorage.”
Apart from her college years in North Dakota, Whitney Miller has spent her entire life in Anchorage, Alaska. “My mom is from North Carolina. She was a military brat who followed my maternal grandfather to Joint Base Elmendorf–Richardson. My dad is from Canada and got a full-ride scholarship to University of Alaska Anchorage.”
PAs were always a part of Whitney’s life in Alaska. “Growing up, everyone I saw for my personal healthcare was a PA,” she says. And a lot of them were graduates of the MEDEX Northwest program. “I rarely saw a physician.” Turns out this had a big impact on her decision to pursue PA as a career path for herself.
For the past three and a half years, Whitney has worked as a medical assistant at Interventional Pain Clinic, a non-opiate prescribing pain management facility. “We did a lot of the steroid injections and other alternatives to get our patients better, allowing them to keep up their normal lives.”
And then there’s been her volunteer work with the No One Dies Alone Program at Providence Health and Services. This unique program is dedicated to providing caring, bedside companionship for dying patients who are alone at the end of life.
To determine her future career direction, Whitney began shadowing both PAs and physicians.
“Honestly, the PAs were really enjoying their time and their lives. And every time I shadowed a physician they would look at me and ask, ‘Why are you becoming an MD? You should be a PA.’ I started to look into it and realized I can do whatever I want to do as a PA, versus an MD. I don’t need a title.”
Now at the start of her PA education, Whitney can look ahead and imagine working anywhere within the State of Alaska. “It just depends on what openings there are and what great opportunities there may be for me,” she says.
“I definitely see the needs in those smaller communities.” Whitney is referring to remote areas that are stressed by the lack of medical providers and services on hand. “I’m interested in rotating through there, and seeing what life is like and where my career will take me.”
Tingrit Desta – Seattle Class 52
 Prior to moving to the United States in 2010, Tingrit Desta worked as a Health Officer (HO) in her native Ethiopia. Equivalent to a PA, the HO profession was developed decades ago by the Ethiopian government as an accelerated medicine program designed to meet the increasing medical needs of the population.
Prior to moving to the United States in 2010, Tingrit Desta worked as a Health Officer (HO) in her native Ethiopia. Equivalent to a PA, the HO profession was developed decades ago by the Ethiopian government as an accelerated medicine program designed to meet the increasing medical needs of the population.
“I worked as a Health Officer for two and a half years, treating patients with HIV/AIDS and TB,” Tingrit tells us. Initially, HO training was available at a few universities within Ethiopia. “Today the program is offered all over the country because MDs are leaving for Europe and the US. Ethiopia is so poor and they cannot pay well. So, the government invests in more training of Health Officers to treat primary care diseases like malaria.”
Once in the United States, Tingrit got her certification as a Certified Nurse Assistant (CNA). During her CNA training at Seattle Community College, her advisor pushed her in the direction of PA education. “I also considered MD, but since the PA program is close to what I was doing in Ethiopia, I got more interested in that. So I started taking prerequisite classes.“
Tingrit worked for five years as a CNA at different retirement homes between New York State and Washington State. “In Ethiopia, I was working with an underserved population—people with a lot of problems like HIV and economic issues,” she tells us. “I really enjoy helping people in need. I think that expresses me. That’s what I really enjoy doing, helping people who really need help.”
Her husband, Yirgalem, was a physician in Ethiopia, and their move to the States required him to study for the US Medical Licensing Examination here. He successfully passed, received his licensure and finished his residency in New York. Eventually, Tingrit and her husband moved west to Port Angeles, WA, where Yirgalem now works at a local hospital as an MD.
Tingrit has now relocated to Seattle to attend MEDEX. Her situation is further complicated by the fact that she and her husband have a 6-month-old child. And how do they manage this?
“Well, Yirgalem works every other week, so he comes to Seattle and spends time with us, then goes back to Port Angeles,” Tingrit explains.
And who’s taking care of her child while she’s in PA education?
“I have a babysitter,” she says with some melancholy in her voice. “The MEDEX Orientation day was my first time away from him in six months. It was hard for me. I didn’t know it would be hard like this. But at the same time, it was a bittersweet moment because I was really excited to join the program.”
Ultimately, Tingrit is focused on the endgame.
“I see myself eventually working in primary care, probably in a smaller city where I can raise my family. That’s my plan.”

Brittany Miner – Spokane Class 22
 Brittany Miner talks about her earliest investigations into a career in the sciences. “Back in elementary school, I thought I wanted to be a marine biologist and work with whales,” she says. “I discovered during marine camp that I didn’t like to touch dead fish very much, but I would love to work with them someday as a side hobby!”
Brittany Miner talks about her earliest investigations into a career in the sciences. “Back in elementary school, I thought I wanted to be a marine biologist and work with whales,” she says. “I discovered during marine camp that I didn’t like to touch dead fish very much, but I would love to work with them someday as a side hobby!”
Perhaps switching gears to medicine would prove more fruitful. At a medical camp at the University of Vermont, Brittany had the chance to learn from medical students and to shadow various medical professionals such as physical therapists, nurses, and doctors. “I went into it thinking that physical therapy would suit me well, but I didn’t get the spark that I thought I would during my shadowing time.”
The only standouts were the physician assistants. “They seemed very calm and very passionate about what they were doing. The autonomy was wonderful. It seemed like a great work-life balance with a lot of options.”
All of this took place before Brittany completed her sophomore year at a Vermont high school. While most people her age are concerned with their social standing in high school, Brittany was planning her future career. We wondered what was behind her drive.

“For a variety of reasons, I was forced to grow up quickly,” she tells us. Working towards a prosperous career would have to come from her own motives. “The way I saw it, I had two options. I could head down a dark road, or I could put my blinders on and go full-speed ahead towards what I want. What I wanted was to truly make something of myself, so that’s what I decided to do.”
Following high school, she worked as a Licensed Nurse Assistant (LNA) at various Vermont residential homes while being enrolled in school. One of her tasks was running the medication cart distributing various medications, narcotics, insulin injections, catheter and colostomy care. “It was wonderful way to start my patient care experience.”
After working at residential homes for a couple of years, Brittany felt she had stopped learning.
“I wanted to be more in the field,” she tells us. “So, I applied as an EMT at a local ambulance service in Brattleboro, Vermont, quickly took an Advanced EMT course, and I worked there for over four years,” she said. “You truly never stop learning.” She also became an ER tech to assist the PAs, NPs, MDs and DOs with a wide array of task-based procedures.
All the while, Brittany was plugging away at her prerequisites for PA school and co-teaching EMT courses. She ended up getting her bachelor’s degree from Southern New Hampshire University, and began the application process to PA schools.

She started applying to East Coast PA programs, but the initial responses were not promising. “I had several friends who were more than qualified to get into PA school, who found out their rejection was largely due to their older age and, surprisingly, their extensive patient care experience,” she said, “I didn’t want to be a part of something that didn’t emphasize the importance of diversity.”
Following her admission to MEDEX, Brittany and her husband, Scott, relocated from Vermont to Spokane for the duration of her PA education with MEDEX Spokane Class 22. “I truly couldn’t be happier to be here,” she says. “Everyone I’ve met has been so wonderful.” Brittany explains how thankful she is for her husband, a paramedic, who has been fully supportive of her throughout this whole process.
When Brittany starts talking about her future career as a physician assistant, her passion is contagious.
“I see myself going into emergency medicine as a PA,” she says, “but I love the freedom of knowing that I can change gears at any point down the road. I have the freedom to develop and change my skills as a provider as my life changes. I just couldn’t allow myself not to have this option!”




