Rural residents travel farther for care and often have more problems accessing care, including medical and surgical specialists, than their urban counterparts. This study compared where urban and rural Medicare beneficiaries received care, how many visits they received, which types of specialists were visited, and how far beneficiaries from different regions and types of areas traveled for care.
We produced two policy briefs. The first compared findings of a similar study conducted by the WWAMI RHRC using 1999 Medicare data from five states (AK, ID, NC, SC, WA). Findings showed that the number of visits by rural Medicare beneficiaries dropped from 9.6 visits per year in 1999 to 8.9 in 2014. The proportion of visits provided by generalist physicians to rural beneficiaries in the five states increased from 29.2% to 41.7% during the same period.
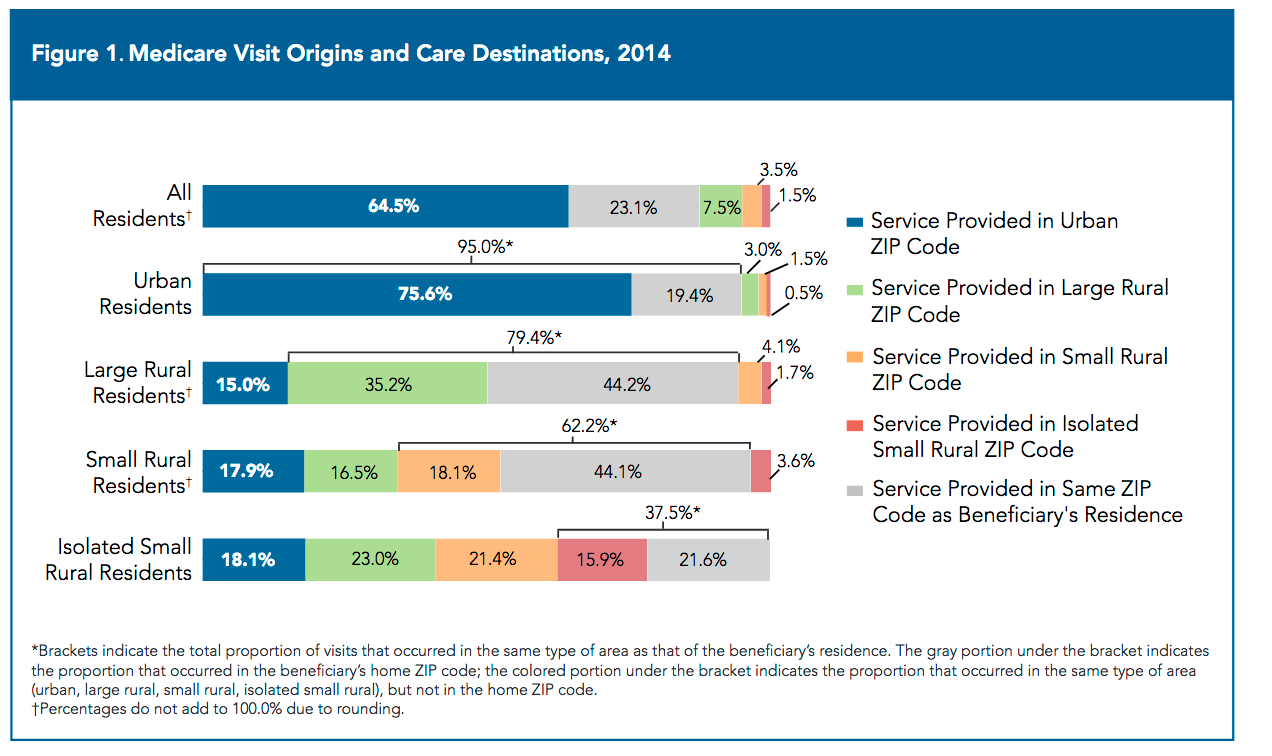 The second policy brief examined national utilization, generalist vs. specialty care visits, and travel time for various types of visits at national and Census Division levels for rural and urban Medicare beneficiaries. Generalist providers (generalist physicians, nurse practitioners and physician assistants) performed over 51.7% of all visits for rural beneficiaries (vs. 38.1% among urban beneficiaries). Rural beneficiaries also had slightly more visits per capita in 2014 than urban beneficiaries overall and within the same Census Division.
The second policy brief examined national utilization, generalist vs. specialty care visits, and travel time for various types of visits at national and Census Division levels for rural and urban Medicare beneficiaries. Generalist providers (generalist physicians, nurse practitioners and physician assistants) performed over 51.7% of all visits for rural beneficiaries (vs. 38.1% among urban beneficiaries). Rural beneficiaries also had slightly more visits per capita in 2014 than urban beneficiaries overall and within the same Census Division.
Beneficiaries from isolated small rural areas, especially Hispanic and Native American beneficiaries, experienced much longer travel times than other rural (and urban) beneficiaries. Over 25% of visits by beneficiaries from isolated small rural areas for serious conditions such as ischemic heart disease and cancer required one-way travel of more than 50 miles, taking more than one hour. The results of both studies underscore the ongoing importance of generalist providers in rural health care and the continuing challenges of access to specialty care posed by the long distances and travel times faced by many rural residents.

