Full Spectrum Family Medicine

Part of our mission is to “…train and empower the next generation of family medicine leaders and educators to provide broad spectrum, team-based care in diverse communities and practice settings.” Our residents are encouraged to explore their interests, learn from broad spectrum family physicians as well as many UW specialists, and practice as broadly as they wish.
Family Medicine Service: Family Medicine resident led inpatient service caring for adult medicine, obstetric, and newborn patients.
Our own Family Medicine faculty teach reproductive health, obstetrics, inpatient medicine, procedures, newborn care, sports medicine, LGBTQ+ care, addiction medicine, and more.
Watch: UWFM Broad Spectrum Training
Watch: UWFM Reproductive Health
Watch: UWFM Behavioral Health
Watch: UWFM Global Health
Watch: UWFM Sports Medicine
Highlights of the Curriculum
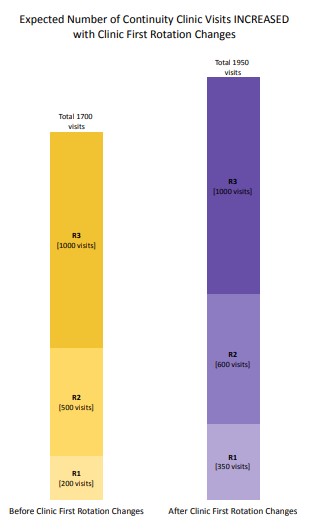
Clinic First
In July 2022 we launched our version of “clinic first.” The goals of clinic first are to improve continuity for residents and their clinic patients; improve patient access; minimize resident time away from clinic to no more than 2 weeks unless on an away rotation; improve resident wellness; and to reinforce that the clinic is where we learn to be family physicians.
We transformed the curriculum to create more time in clinic for residents, especially during the R1 and R2 years. Mini-blocks in some of our more inpatient heavy rotations will allow concentrated clinic time that is free from inpatient responsibilities. Resident schedules will be more predictable allowing for return visits for patients who need them.
We will measure continuity and access to ensure that we are meeting our intended goals and check in with residents and faculty to evaluate the new changes.
Diverse Training Sites
- Rotations at UW Medical Center, Harborview, Northwest Hospital, Seattle Children’s Hospital, Veteran’s Administration, and many other community sites
- Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI) opportunities – experience the five state region during elective rotations
Collaborative Learning
- Learn from FM residency faculty, FM
department faculty, and faculty from many
other specialties across UW - Work with incredible resident peers within
the residency and across UW - Behavioral Health: addictions clinic, BHIP,
consulting psychiatrist in clinic - Fully integrated into general surgery and ICU as a fellow resident with the same expectations and opportunities
Areas of Concentration
- Recent AOCs include Sports Medicine, musculoskeletal medicine, clinician educator, global health, integrative medicine, mental health,
reproductive health and abortion, and
quality improvement - Endless options for electives and AOCs
An Area of Concentration (AOC) is a framework for family medicine residents who elect to pursue more advanced, in depth training in an area of choosing, with the goal of gaining additional skills and knowledge for future practice or career steps. It is specifically intended to be a “stretch” goal during normal residency training, NOT additional time or a fellowship, individualized to meet the needs of the resident.
The concept of focused training has been part of family medicine graduate education for decades. Many of us have expertise in specific areas of family medicine that we have developed on our own. This expertise not only can enhance patient care outcomes, but also can lead to sharing of skills and resources with colleagues and learners via teaching or other scholarly work.
The overall goals are to provide an opportunity to recognize a resident’s extra efforts; encourage and recognize scholarly activity and presentations; encourage resident participation in national meetings; provide a framework to showcase areas of excellence; and help applicant students identify programs that meet their specific needs.
The requirements for an AOC are:
- A written program of study designed by the resident with faculty input that identifies the area of study with competency-based goals and objectives and an evaluation component.
- At least 2 months or 200 hours of training in the AOC, above and beyond RRC requirements.
- A scholarly project completed in the AOC, which should be presented and evaluated locally. Presentation at the state and/or national level is encouraged.
- Attendance at a national CME meeting in the AOC.
- Journal club (critical appraisal) presentation of an article in the chosen area.
- Quality outcomes must be demonstrated, using case logs with patient outcome data, procedure logs and faculty reviews of resident competency in the AOC.
- Successful completion of the residency program itself.
The AOC should be documented through a portfolio of materials that include the above.
Ideally, an AOC should be identified and started by the R2 year, although development in the early R3 year is acceptable if requirements can still be met by graduation. The initial steps are to identify an area of interest, and a faculty mentor who agrees to work with the resident in that area. The resident is responsible for submitting the plan for the AOC in the format attached; developing the portfolio; and completing the requirements. A certificate will be presented at graduation acknowledging the completion of the AOC, and will be included in summary evaluations of the resident sent to future employers.
Examples of recent AOCs include:
- Musculoskeletal Medicine
- Reproductive Health
- Sports Medicine
- Scholarship and Research
- Clinician Educator
- Quality Improvement
- Global Health
What is a RHEDI program (Reproductive Health, Education in Family Medicine)?
- UWFMR is a RHEDI program. As such, abortion and contraception training are integrated into the curriculum. All residents will gain exposure to abortion care (medication abortion, procedural abortion, post-procedure care, pregnancy options counseling) and contraceptive care (includes IUD/implants insertion and removal, vasectomy counseling). Residents may opt out of clinical abortion training, though residents cannot opt out of didactics on abortion or decline to go to required training sites, including Planned Parenthood. Abortion care is integrated into our primary care clinics at Northgate and Harborview.
- We also teach and employ a reproductive justice (RJ) framework into all aspects of the Sexual and Reproductive Health (SRH) curriculum. Residents learn to identify and resist longstanding patterns of racism and white supremacy that profoundly shape contemporary medical practice, and SRH in particular. We discuss and model respectful and equitable abortion and SRH provision for LGBTQIA+ people and people with disabilities.
- Residents with special interest in SRH skills may consider completing an Area of Concentration (AOC) in SRH and/or apply to obtain additional training in abortion procedures or vasectomy procedures through local and national elective rotations.
- All of our residents will learn:
- Non-coercive, non-judgmental, patient-led contraception counseling
- Management of patients who are using all forms of pregnancy prevention, including LARCs
- Patient centered counseling for patients with a positive pregnancy test, including non-coercive, non-judgmental options counseling
Point of Care Ultrasound
Recognizing the growing nationwide momentum of POCUS use in primary care, the UWFMR devised and started a contemporary, longitudinal POCUS curriculum to span the three years of residency training.
POCUS – Point-of-care ultrasound (POCUS) is a rapidly growing area of interest within primary care and is sometimes referred to as the “stethoscope of the 21stcentury”. When utilized appropriately by a trained clinician, POCUS can answer a specific clinical question or provide immediate diagnostic information in real time, and it has many potential applications. Recognizing thegrowing nationwide momentum of POCUS use in primary care, the UWFMR devised and started a contemporary, longitudinal POCUS curriculum to span the three years of residency training. Skills will be introduced in the first year of residency and expanded upon throughout years two and three. The curriculum includes individual, small group, and large group teaching and workshops. Both the Northgate and Harborview clinic sites have state-of-the-art ultrasound machines both for clinical use as well asthese educational initiatives. This is an area ripe for scholarship and clinical research for interested residents.
Procedures
We strive to care for as many patient needs as we can in our clinics and hospital services. Part of this effort is providing indicated procedures.
Examples of procedures:
- Outpatient procedures
-
- Skin: biopsies (punch, shave, excisional biopsies), cryotherapy, dermoscopy, laceration repairs.
- Lumps and bumps: I&Ds, lipoma and cyst excisions
- MSK: joint injections and aspirations, ultrasound, casting and splinting
- Reproductive health: IUD and Nexplanon insertions and removals, terminations (medical and surgical), endometrial biopsies,colposcopies, vasectomies
- Newborn: circumcisions
-
- Other: thrombosed external hemorrhoid treatments, tongue tie release, anoscopy
- Inpatient procedures
-
- Vaginal deliveries
- CVC and arterial line placements
- Lumbar punctures (adult and pediatric)
-
- Thoracentesis, paracentesis
- Fracture reductions
- Colonoscopies
- C-section assist
- Intubations
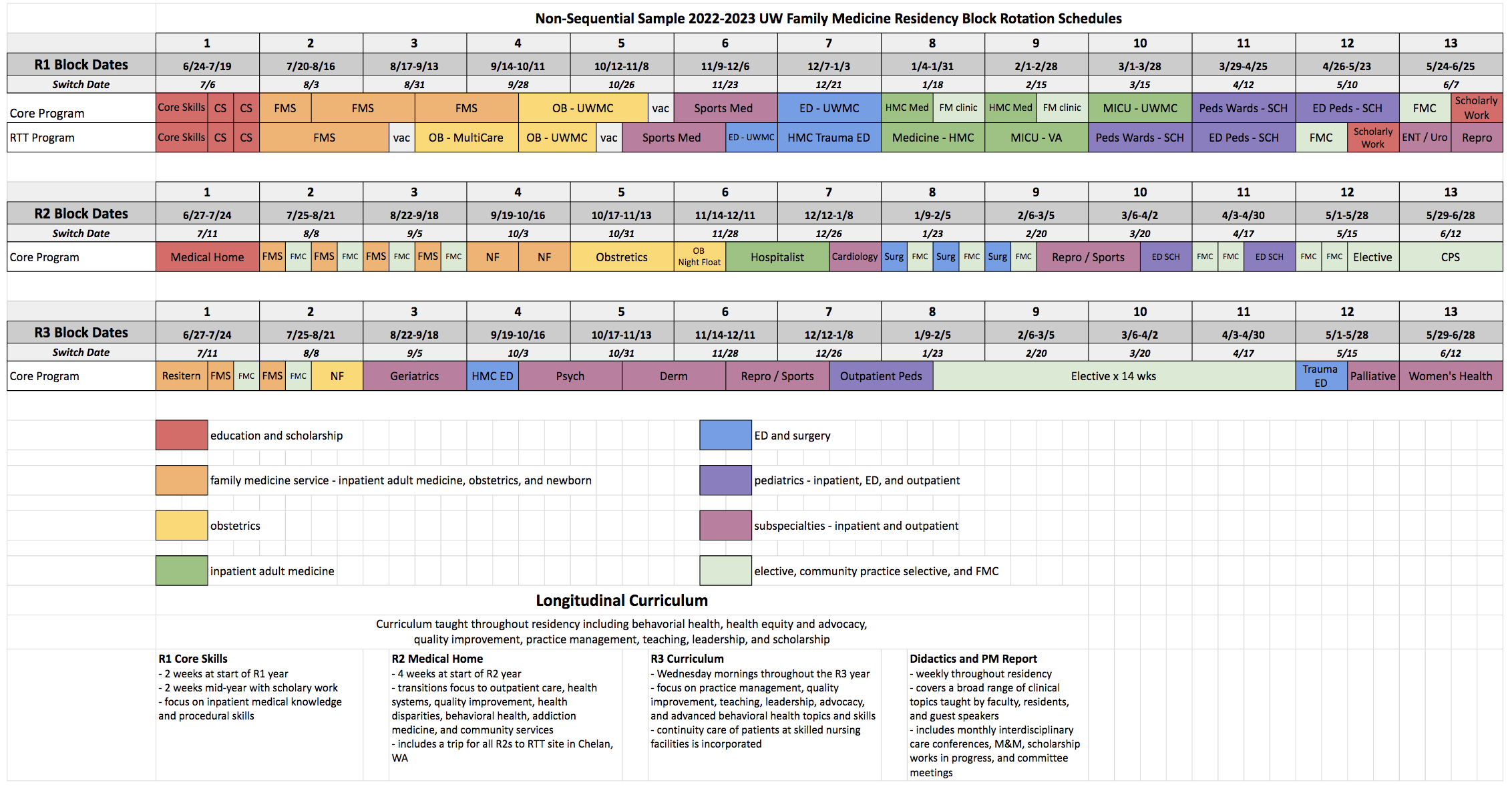
*Please note these are sample schedules.