Friends and Colleagues: After a snowless winter on the west side, it is finally springtime. The cherry blossoms on campus have come and gone, and we have received our match results—both true harbingers of the season. I am glad to see Spring arrive, because this Winter was a hard one for us. In my January Chair Notes, I began by writing about the loss in December of Roger Rosenblatt. On February 27 we lost another friend and long-time Professor in our Department. Stuart Farber, MD died after a long battle with leukemia. I first met Stu in the late ‘80’s, when I was Program Director at Tacoma Family Medicine. As a family physician practicing in Tacoma, Stu regularly served as a preceptor for our residents; he believed strongly in the importance of medical education. One of his strong interests was providing high quality end-of-life care, and he spent much time teaching the residents about this topic. After helping to start the Hospice of Tacoma, Stu took a sabbatical to learn more about the then emerging field of Palliative Care. Upon his return he focused on this new and critically important area of medicine. He came to UW and worked in our Department, while developing one of the first educational programs in Palliative Care for medical students. His passion for quality care in this area resulted in his leadership in creating a Palliative Care Consultation Service at UW Medical Center. Several years ago Stu was diagnosed with leukemia and recognized that the disease would probably eventually take his life. Following his own teachings, he served as an exemplar for all of us by planning carefully, prioritizing thoughtfully, and re-telling his story during the last years. Stu’s loss will be felt by all of us. During the last part of his life Stu and his wife Lu initiated efforts to create the Farber Endowed Professorship in Palliative Care. When completely funded, the Professorship will memorialize Farber’s legacy of teaching students and residents the art of providing good care at the end of a patient’s life. If you are interested in supporting the Professorship, go to https://depts.washington.edu/givemed/give/?source=farpro.
National Perspective: Since we last met I have attended the board of directors meeting and the annual meeting of the Association of Departments of Family Medicine (ADFM) and the ABMS Board Retreat. Key topics at ADFM included. . . .
Hope Wittenberg, Director of Government Relations for STFM and ADFM updated us on activities of the Academic Family Medicine Advocacy Committee (AFMAC). This is a group of the four members of CAFM plus the AAFP. The active advocacy topics for AFMAC include:
- Federal GME Funding (Top Priority) (with Teaching Health Centers high on the list)
- Workforce—including residency position, expansions, funding and medical school expansion
- Title VII
- Research, including developing a federal funding stream for FM through PCORI and support of AHRQ
- Family Medicine for America’s Health (academic issues related to federal policy
Other issues Hope mentioned:
- The President’s FY16 budget reduces non-defense spending. The potential impact on 2016 spending is that AHRQ, Title VII, NIH, CDC funding are all at risk and will need to be specifically funded.
- Debt Ceiling—will need to be raised again to prevent government shutdown
- “Primary Care Cliff”: This is a name being applied to the fact that mandatory spending on a number of programs important to FM is set to expire at the end of this fiscal year. This group includes community health centers (1/2 of funding expires), NHSC (all funding set to expire), Teaching Health Centers (all funding expires).. To reverse each of these, specific action by Congress will be needed.
- Primary Care Incentive Payments—run out at the end of this calendar year
- Title VII grew to $38.9M last year and another $39M is in the President’s budget this year.
- Medicare GME: As a specialty, we are interested in global GME reform. The President’s budget is the same as last year, with a proposed IME (indirect medical education) cut of 10% for deficit reduction, competitive grants for THC and children’s GME, as well as a discussion of 13,000 new slots for shortage specialties. The good part of this is that this will stimulate conversations on GME. It is anticipated that several years of conversation will be needed before any significant action is taken.
- Teaching Health Centers: Regarding the major issue of funding for THC’s, Hope reported that there is some hopeful news on the horizon. There is currently a move to move THC funding to CMS. This is being considered by the House Health Committee. More information should become available within the next couple of weeks.
- Hope noted that this large group of issues will probably result in urgent calls from her office and the AAFP to contact our legislators. She feels that it will be very important for us to respond to these this year.
At ADFM Jim Puffer (CEO of ABFM) and Carlos Jaen (Board Chair of ABFM) discussed the recent moves by the American Board of Internal Medicine to put their version of Maintenance Of Certification (MOC) Part IV on hold. There is very good evidence that for Family Physicians, participation in Part IV of MOC improves the quality of their practices and the outcomes for their patients. On another topic, Jim and Carlos commented on ongoing concerns about the scope of practice of Family Physicians. ABFM is studying what appears to be a decrease in hospital care, a decrease in procedural care, a decrease in pediatric care, and a decrease in maternity care by Family Physicians. Is this really happening? Is it happening to all family doctors at the same time, or does it happen to us individually as we age? Is it the same for physicians practicing in small towns as it is in large cities? Many questions exist. Jim and Carlos also reported on the ABFM pilot project to datamine the E.H.R.’s of family doctors to see how they actually practice. This might eventually replace some parts of the MOC exams.
On a different topic, the ABMS Retreat focused on the challenges that our specialty boards and the MOC programs are facing. If you have not read the opposing PERSPECTIVE articles in the January 8, 2014, New England Journal of Medicine, I recommend doing so. We need to support the efforts of ABFM and the other Boards to continue legitimate certification programs. The issues involving ABIM do not seem relevant to ABFM.
As I write this column, the House has passed a bill to permanently fix the Medicare Sustainable Growth Rate. The Senate is in recess for two weeks, but it is hoped that they will pass the bill with they return, and we will finally see an end to the short-term “patches” that have been passed for many years. It is also hoped that this bill will include funding for several other items important to Family Medicine. Stay tuned.
Medical Student Education (MSE): Our medical student education program continues to be very busy. Over the last two years, as the curriculum renewal project has been underway, we have been working hard to be sure that Family Medicine maintained a significant role. I am pleased to report that this has happened, and a number of Family Physicians are involved. The new curriculum will teach the entire first 18 month Foundation Phase at our previous first year sites, including Seattle, Spokane, Moscow, Bozeman, Laramie, and Anchorage. Each of these sites will feature an 18 month long Primary Care Clinical Practicum, with students spending time each week in a primary care (mostly Family Medicine) practice. This is envisioned as a continuity experience with the same primary care precepting physician and practice for the entire Foundation Phase. The highly popular Rural Underserved Opportunities Program (RUOP), long supported by WAFP, will continue. The Targeted Rural Under-Served Track (TRUST) has grown and will soon be available to students from all WWAMI states. Family Medicine faculty are leading several themes in the curriculum, including Diversity, Lifelong Learning and Health Equity. Our career advising program has been very active, and I am very pleased to report that 34 UW senior medical students matched into Family Medicine residencies. This represents 16% of the graduating class, with 65% of these future family physicians matching into residencies in the WWAMI states.
UW Family Medicine Residency: Spring is a busy season in residency education. The R-3’s are preparing to enter practice, and the program is anticipating the arrival of new R-1’s. It is always a bittersweet time with hellos and goodbyes. Our residency program filled with great new R-1’s in the match. The new graduates are from the University of Minnesota, Creighton, Emory, UCLA, University of New Mexico, USC, UCSF, and UW. Major projects over the last year have included preparation for ACGME’s Next Accreditation System and work on the new “milestones” residency evaluation system. Jo Jackson, MD, one of our long-time faculty members is retiring, and we have hired Kim Collins, MD, one of our Harborview graduates who had been in practice in Snohomish, to join us.
Fellowships: We are now offering several fellowships at the R-4 level. These include our Chief Resident position, ACGME-accredited Sports Medicine and Palliative Care fellowships, and a non-accredited self-sustaining Global Health fellowship; all of these positions have filled.
UW WWAMI Family Medicine Residency Network: In conjunction with the WAFP, the WSMA, and others, the Network has been advocating at the Washington State Legislature for improved Family Medicine GME funding for Washington residencies. We probably will not know the outcome of this effort until the end of the legislative session. We hope to increase funding to at least the level that we had prior to the recession. I sincerely appreciate WAFP and WSMA advocacy support for this effort. Two other major projects in the Network are supporting new residencies and offering our help to the osteopathic Family Medicine Residencies as they prepare for the new ACGME unified accreditation system.
MEDEX Northwest Physician Assistant Program: MEDEX now has three first year sites in Washington—Seattle, Spokane, and Tacoma—as well as the site in Anchorage. The newest site is Tacoma. It focuses on training veterans, and it will graduate its first class this summer. The second year MEDEX clinical students participate in rotations all around the region. Otherwise MEDEX is doing well. We are continuing our search for a new leader of the program.
Sports Medicine: We have 5 faculty members who practice at the Stadium Clinic and who support both the Husky athletes and the SeaHawks. This group focuses their research on tendon pathology, concussions and heart problems, including sudden death, in young athletes. Jonathan Drezner, MD has successfully established the Center for Sports Cardiology at the Stadium clinic.
Palliative Care: The newest section in the Department is Palliative Care. Both the UWMC Palliative Care program and our medical student education program in Palliative Care were started by Stu Farber, MD. As noted in the introduction, Stu died last month, and while we will all miss him, his gift to us is UW Medical Center’s outstanding end-of-life program and the education of hundreds of medical students in this important area of our care. Lu Marchand, MD is now leading our Palliative Care group, which is steadily growing and serving more patients.
Research:
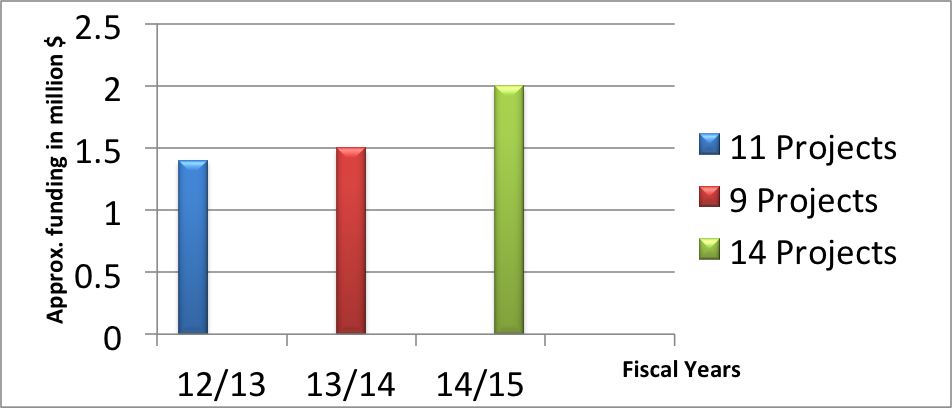
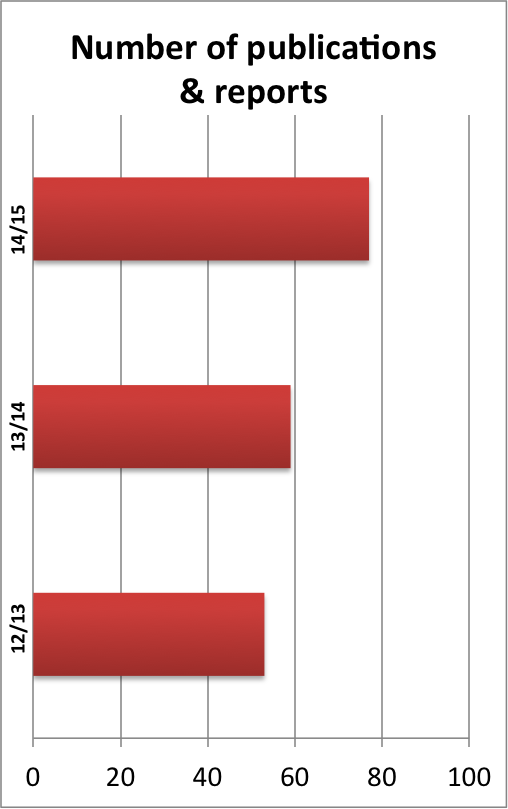
With the addition of our new federally funded Center for Health Workforce Studies, the Research Section is growing. These graphs illustrate our growth in both publications from the Section and grant funding:
Summary: Overall, the University of Washington Department of Family Medicine is doing very well. Our success would not be possible without your support and without the “Family Medicine friendly” climate in the Northwest. Our Department has more volunteer clinical faculty members than any other department at UW. You are the people who help us succeed in our decentralized education and research efforts. Thank you for your ongoing support.
Tom E. Norris, MD
Professor and Chair
