[box title=””]Bianca K. Frogner, PhD
Director of the Center for Health Workforce Studies
Associate Professor, Department of Family Medicine
School of Medicine at University of Washington
bfrogner@uw.edu
Suggested reference:
Frogner BK. How many health care workers are at risk of being sacrificed to COVID-19 in the US?[Internet Blog] Center for Health Workforce Studies, University of Washington, Mar 31 2020. http://depts.washington.edu/fammed/chws/how-many-health-care-workers-are-at-risk-of-being-sacrificed-to-covid-19-in-the-us/[/box]
Introduction
Health care workers are the heroes of the coronavirus disease (COVID-19) pandemic and the soldiers working on the frontlines caring for patients while also being at risk of catching the virus and sacrificing themselves. In China and Europe, health care workers have died and thousands more are out of commission due to self-isolation. An increasing number of stories are sounding the alarm that heath care workers in the US are getting sick and may die from COVID-19, and no one is tracking these numbers. Health care workers worldwide are facing unnecessary risk because of a shortage of screening tests and personal protective equipment (PPE).
What has yet to be estimated is how many health care workers are at risk of getting sick and dying from COVID-19 in the US. These questions are difficult to answer due to the many assumptions about the true incidence and prevalence of COVID-19 seen in clinical environments and the unknown spread rate of the disease among the health care worker population. In this blog, I aim to answer these questions with the goal of stressing the urgency to screen all health care workers, ensure distribution of PPE across a broad range of health care settings and occupations, and track this unfortunate occupational hazard. I find that nearly one in six health care workers may be at risk of testing positive for COVID-19 and up to 380,000 deaths if we emulate the experience of Italy.
Identifying Health Care Workers at Risk of Being Infected by COVID-19
Not all 16.5 million health care workers are on the frontlines of the COVID-19 pandemic. The type of workers on the frontline, such as medical assistants, is rapidly changing as outpatient clinics and offices of physicians close to concentrate their efforts on emerging COVID-19 patients and prevent infection of others.
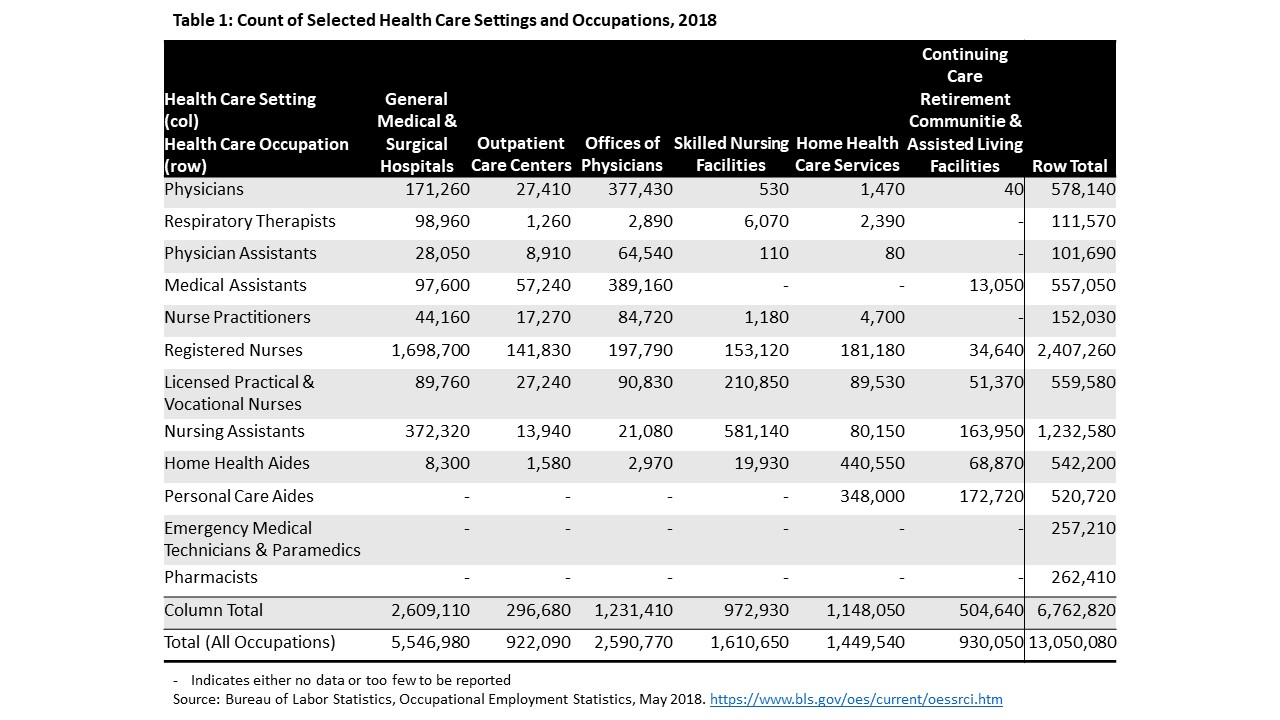
I selected six clinical settings and twelve health care occupations identified using the Occupational Employment Statistics collected by the U.S. Bureau of Labor Statistics that are most likely to be on the frontline of the COVID-19 pandemic (Table 1). Not all of the workers in these settings provide direct patient care but rather provide support services such as food preparation, custodial care, and insurance processing. Working in these environments, still place these workers at risk of contracting COVID-19 and they may require testing and protection. Of the twelve selected occupations, ten of these occupations primarily work in one of the six settings. Two additional occupations–EMT/paramedics and pharmacists—are considered in the analysis given their importance to the frontline of the pandemic. These workers are more likely to be found in the community setting rather than a clinical setting.
Estimating COVID-19 Positive Test Rate and Case Fatality Rate among Health Care Workers
Rates reported are from the most recent data available – March 30, 2020 – unless otherwise noted.
Positive (Confirmed) Case Rate
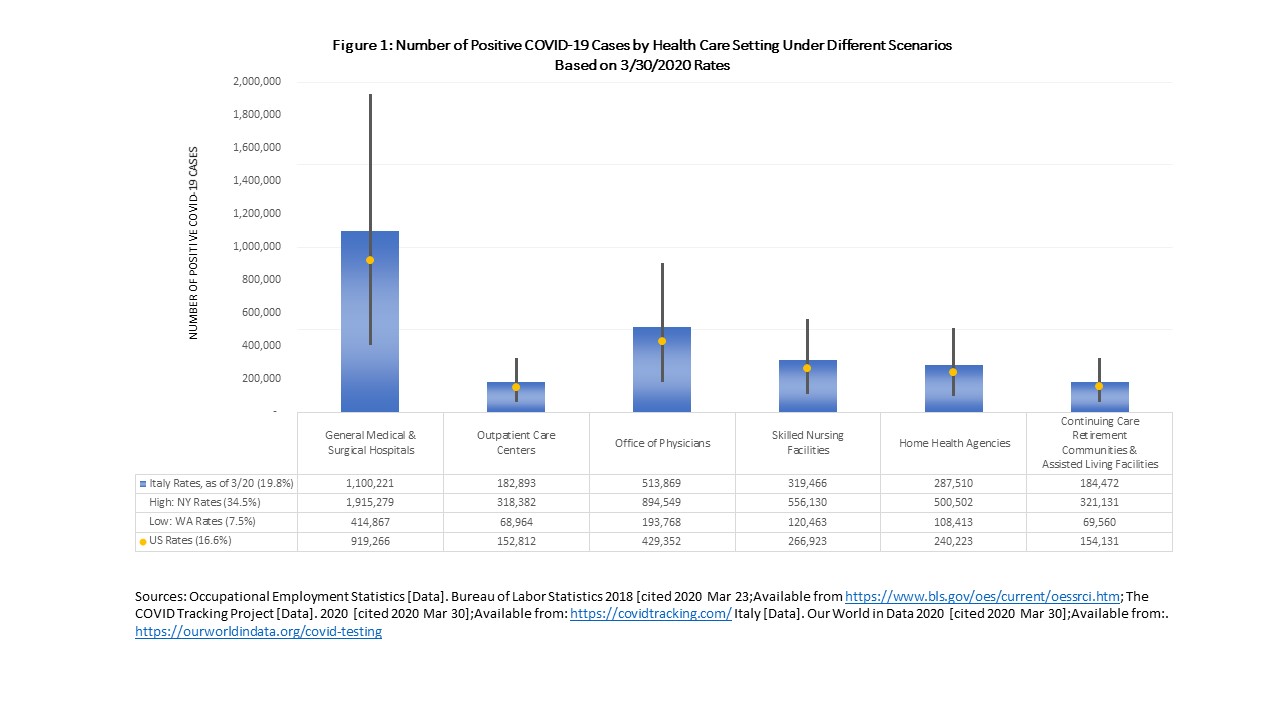
At this time, we do not have any national estimates on the infection or mortality rates among health care workers in the US. All 50 states and the District of Columbia have reported at least one case of COVID-19, yet not all health care workers are exposed to COVID-19, let alone tested. For this calculation, I assumed that all health care workers are at risk of being infected to COVID-19 and will eventually be tested for the virus. Data from the COVID Tracking Project was used to estimate the positive (confirmed) COVID-19 case rate in the US among those tested. The confirmed cases are ever evolving as more tests are made available across the country. The US rate is slightly higher than one report of COVID-19 infections among physicians and nurses in a hotspot in Italy.
To get a high and low estimate with in the US, I used Washington state as the lower bound rate because Washington has been testing for the longest time in the US due to having the first confirmed COVID-19 case and it has conducted the second highest number of tests behind New York. I used New York State, which has conducted the largest number of screening tests and has the worst outcomes of any state, as the upper bound rate. For comparison, I applied the rate of confirmed cases in Italy where testing has been widespread and going on for longer than the US.
Case Fatality Rate
Like confirmed cases, the estimated case fatality rate, or the number of deaths among confirmed positive cases, in the US is also rapidly changing with more testing. I drew from two reputable sources for case fatality rates: Centers for Disease Control and Prevention (CDC) and Johns Hopkins University (JHU). Again, for comparison, I used Italy’s case fatality rate to give a sense of the potential trajectory if we do not get COVID-19 under control and protect our health care workers. The true case fatality rate depends not only on how many people get tested but also whether there may be bias in who is getting tested.
The testing rate and death rates are likely to be based on those who are showing symptoms, which may skew the rates higher than if we were to look retrospectively at the impact of COVID-19 on the entire population. We know, however, that the case fatality rate is higher among the elderly and possibly among males; demographics of the health care workforce alone do not necessarily put them high risk given they are not older than the general population – though this varies by profession and across regions – and they are more likely to be female.
Which Health Care Settings May Experience the Greatest Loss?
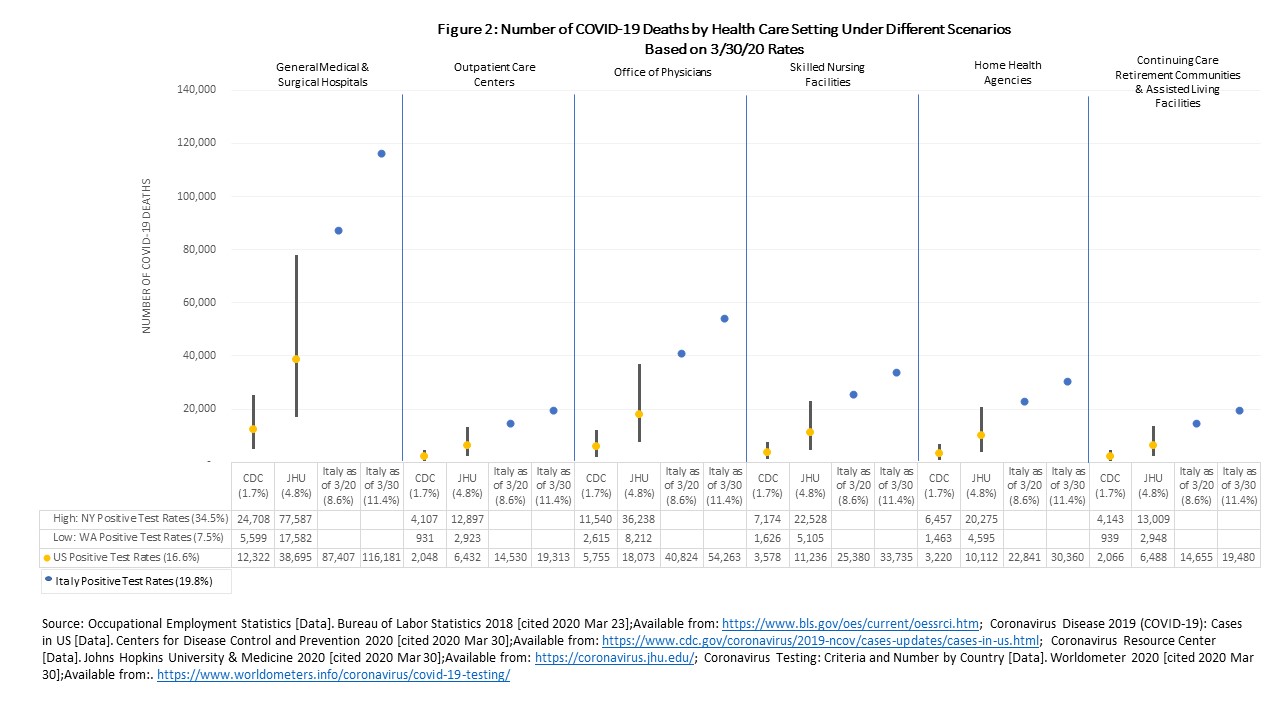
The six settings represent 78% of the total health workforce, hospitals being the largest health care employer. Given the size of its employee base, hospitals will likely experience the greatest number of positive cases (919,266 and ranging from 414,867 to 1.9 million based on Washington and New York state rates, respectively) and greatest number of deaths (15,690 based on CDC case fatality rates and 44,069 based on JHU rates) (Figure 1 and Figure 2). Long-term care settings including skilled nursing facilities, home health and continuing care and assisted living facilities are where patients are the most vulnerable and the community spread has been concentrated. When combined, the number of positive cases across the three settings are estimated at 661,277, ranging from 298,436 to nearly 1.4 million, and the number of deaths estimated at 11,287 using CDC rates and 31,702 using JHU rates.
Which Health Care Occupations May Experience the Greatest Loss?
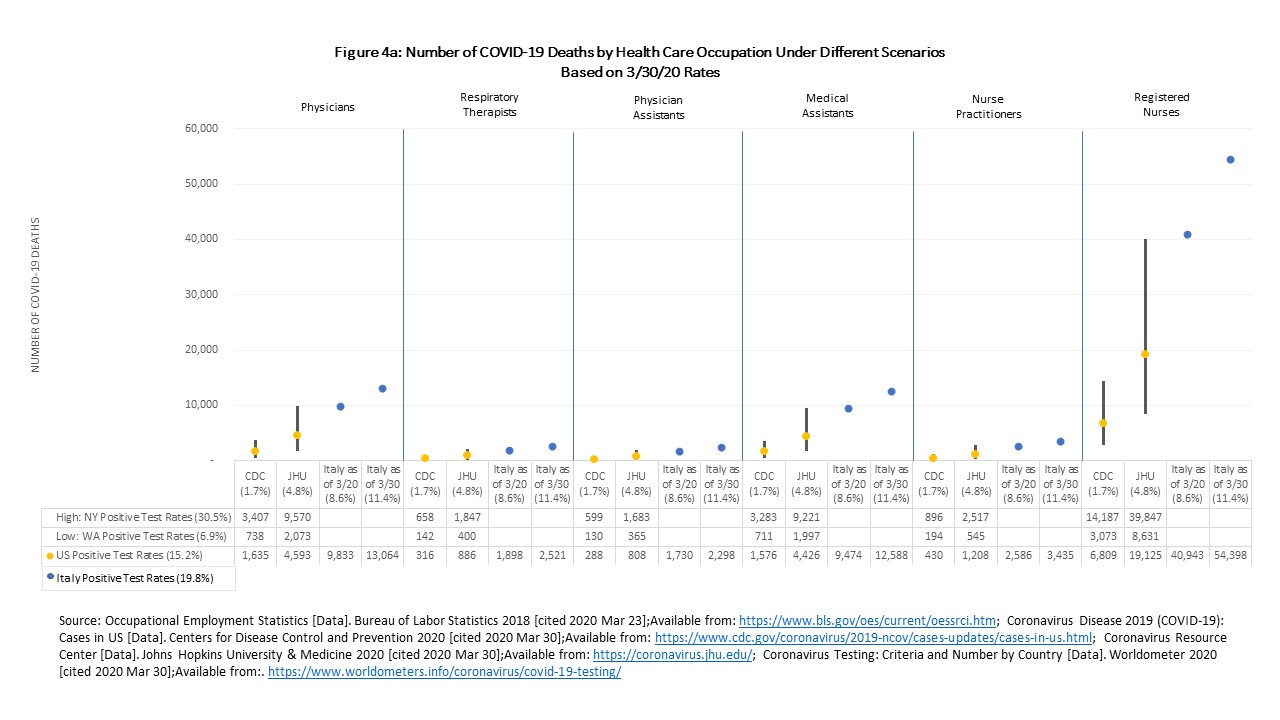
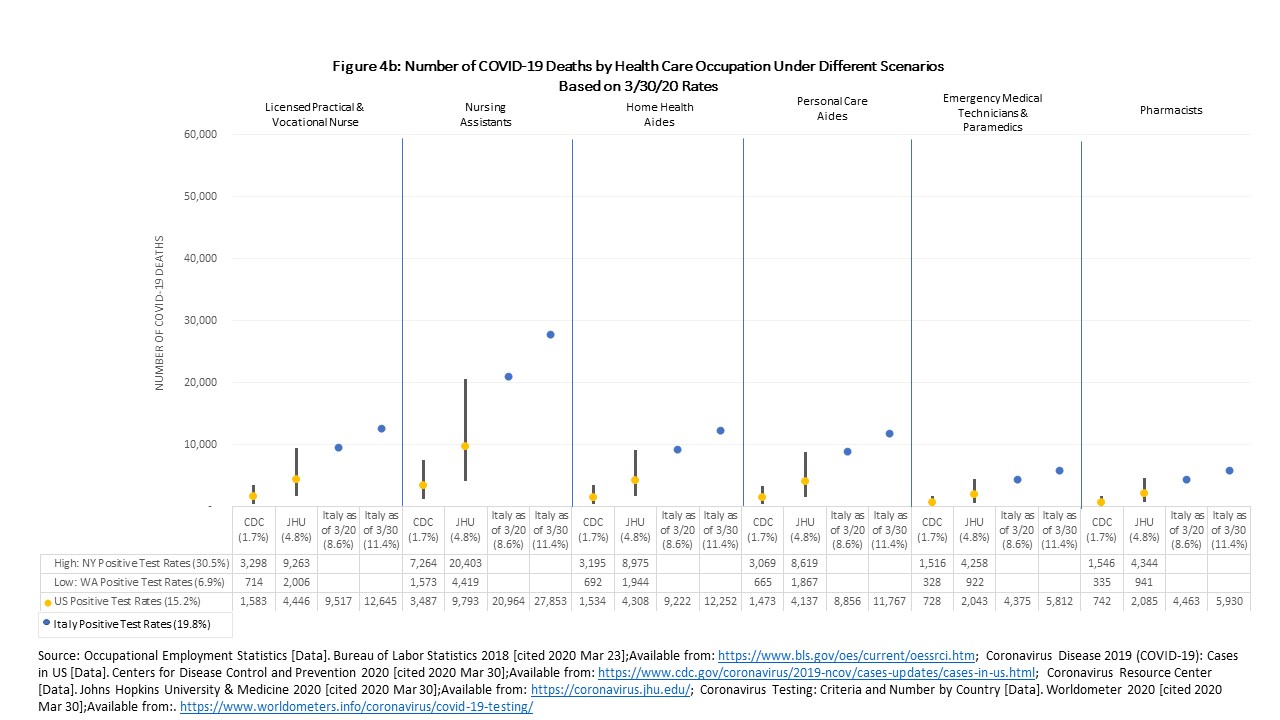
Registered nurse is the single largest occupation in health care, representing about 18.0% of our pool of health care workers. Given the size of this workforce, they are also the ones who may suffer the greatest number of COVID-19 cases and deaths with nearly 400,000 positive cases and 6,809 to 19,125 deaths estimated (Figure 3 and Figure 4a). Nursing assistants, the second biggest occupation, may see nearly 200,000 positive cases and 3,487 to 9,793 deaths (Figure 4b). These two occupations are also most often working in settings that are experiencing the highest risk of COVID-19: hospitals and skilled nursing facilities. Physicians, who are a critical segment of the workforce and may be tough to backfill given the length of training, may see 95,812 positive cases and 1,635 to 4,593 deaths.
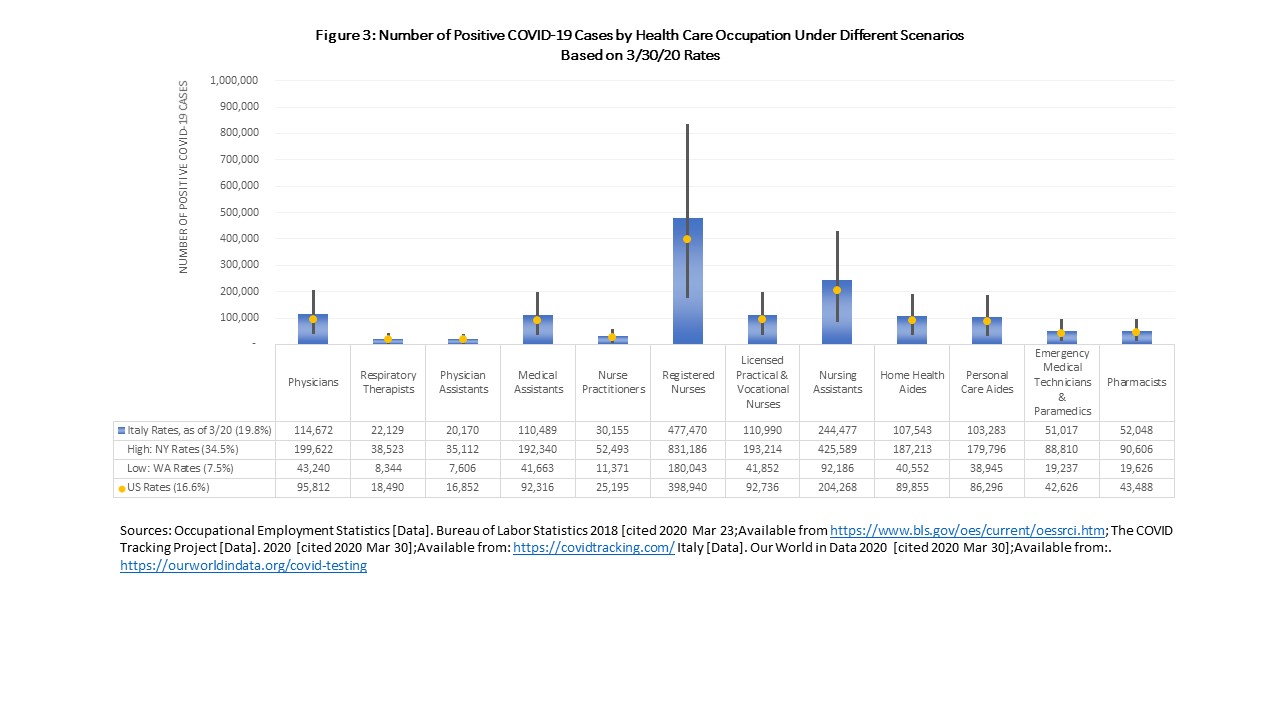
Home health aides and personal care aides (often called direct care workers) may see a combined 176,151 positive cases and 3,007 to 8,445 deaths. Direct care workers are among the most vulnerable including having poor physical and financial health compared to other health care workers and is a workforce already experiencing a shortage before the COVID-19 pandemic. Generally, health care workers may have better access to health care and thus may be able to get care sooner than the average patient, but many of our aides and assistants are least likely to have PPE and they receive inconsistent training to protect themselves.
Overall View of COVID-19 Effect on Health Care Workforce
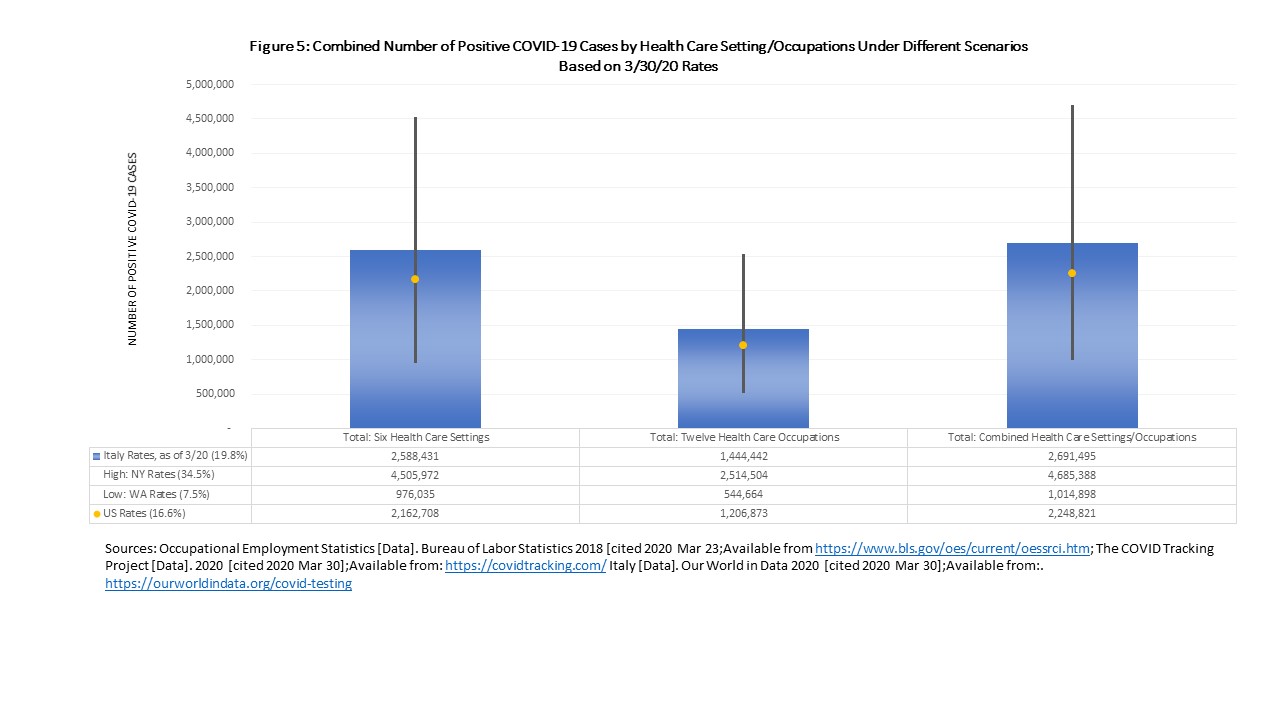
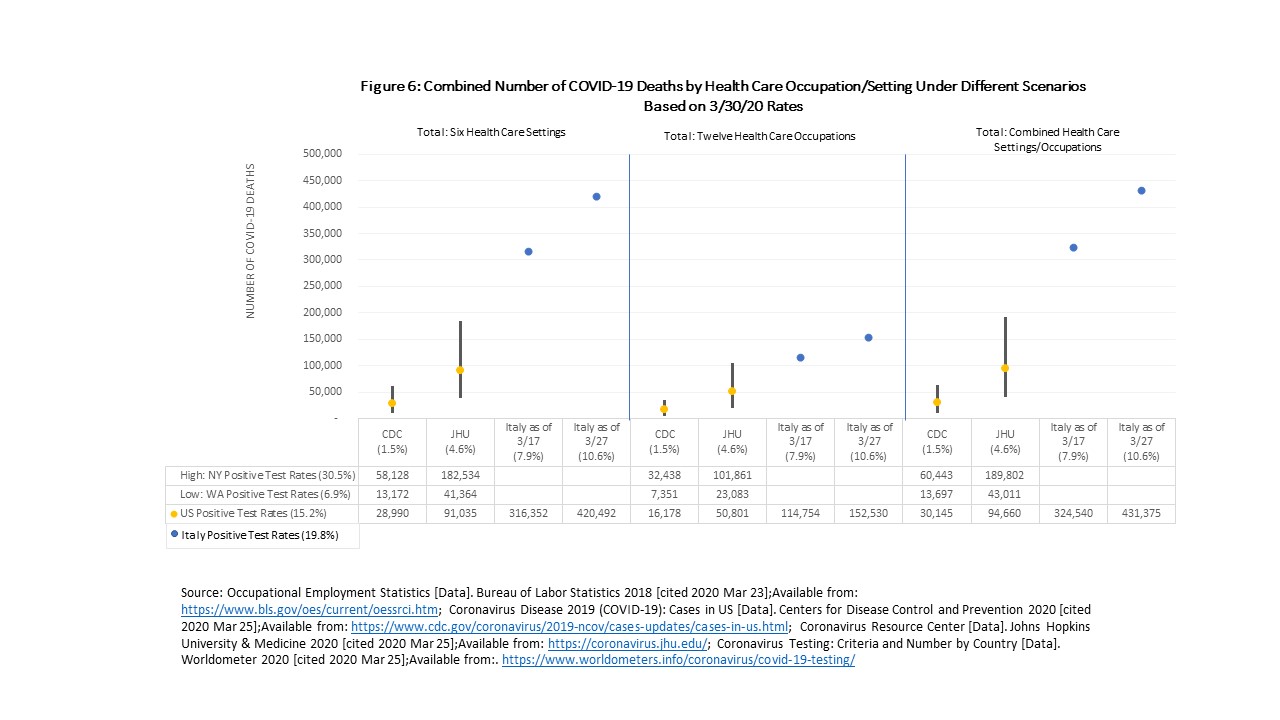
Of the 13.6 million health care workers assumed to be on the frontlines of COVID-19, I estimate that 2.8 million will be tested positive assuming a rate of 16.6%, with a range of 1.2 million based on Washington state rates to 5.8 million based on New York state rates (Figure 5). The range of deaths could be as low as 21,436 up to 277,957, nearly a 13-fold difference, using US-based rates (Figure 6). If the US does not get control over COVID-19 and our country follows Italy’s course, deaths could reach almost 380,000. Specifically, among the twelve occupations, 1.2 million are estimated to test positive with COVID-19, ranging from 0.5 million to 2.5 million; 20,599 to 57,857 may die, with a range from as low as 9,297 up to 120,545 using US-based rates. Counts will vary for occupations based on differential exposure to patients which can make the numbers go up and availability of PPE which can make the numbers go down.
Conclusion
Based on other countries’ experiences, health care workers have been among the bulk of positive COVID-19 cases. We need to protect all of our health care workers, especially those at the frontline, because losing any of them means many COVID-19 patients will not receive the care they critically need. Protecting our health care workers means giving them the tools and gear they need to fight the virus. Losing any lives to the pandemic is devastating and society will be put at greater risk of losing more if we unnecessarily sacrifice health care workers lives by not given them the protection they need.